Sites of Secondary Breast Cancer
If you or a loved one is dealing with secondary (metastatic) breast cancer it can be very overwhelming, especially if you’re still learning about what is actually happening inside your body. This page is here to provide information about where in your body secondary breast cancers most commonly spread to.
You can also find information about the specific symptoms associated with each site, and the most common treatments for each site. Learning about what is happening inside your body as a result of your secondary breast cancer can be empowering and can help you and your clinical team work together effectively. They will be able to give you personalised information about the treatment options available to you. Thanks to research, treatments have improved in recent years and people with secondary breast cancer are living longer with a better quality of life after their diagnosis.
On this page you will find:
What is metastasis?
Primary breast cancer becomes secondary breast cancer (also known as advanced breast cancer, stage 4 breast cancer and metastatic breast cancer) when cells from the original tumour break away and travel to different sites in the body. This is called metastasis. The cancer cells travel through the bloodstream or the lymphatic system and “land” in certain places. New tumours may then grow at these new sites.
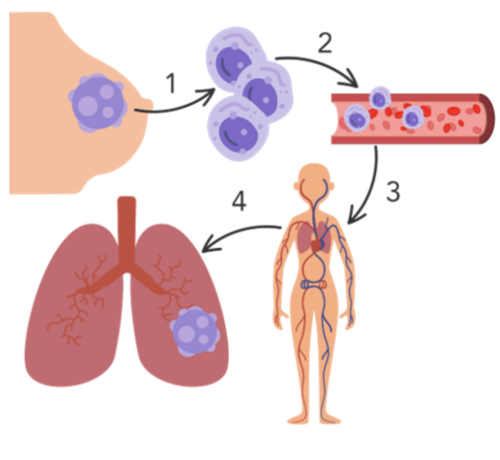
Figure 1. The metastatic pathway: 1) Cancer cells detach from the primary tumour site and invade the surrounding area of normal tissue 2) cancer cells invade the blood or lymphatic system 3) cancer cells travel through the blood or lymphatic vessels to reach target sites 4) cancer cells exit the blood or lymphatic vessels and form a secondary tumour at the target site e.g. the lungs.
Once cancer cells reach a secondary site, they do not always turn into aggressive tumours, they may stay inactive for a while, or permanently.
The five most common sites of metastasis for secondary breast cancer are: the bones, brain, liver, lungs, and skin.

In the Bone / In the Brain / In the Liver / In the Lungs / In the Skin
Secondary Breast Cancer in the Bone
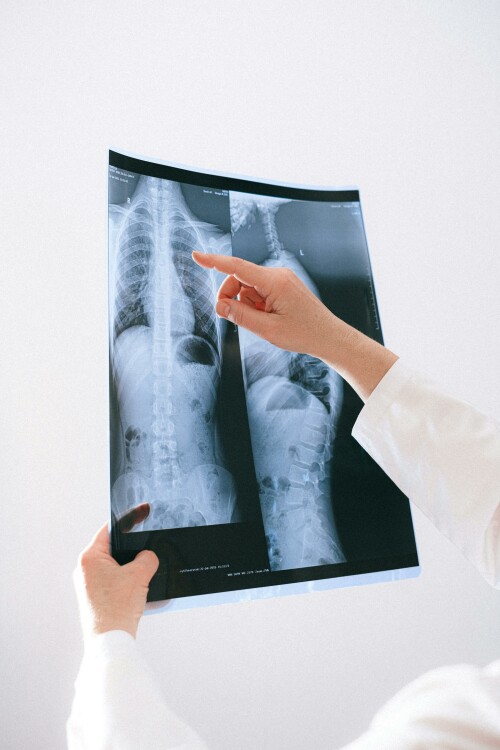 When breast cancer cells spread to the bone, it is commonly referred to as bone metastases, bone mets, or lesions. The primary cancer cells that have spread to the bones are breast cancer cells, so this is not the same as having cancer that originates in the bone.
When breast cancer cells spread to the bone, it is commonly referred to as bone metastases, bone mets, or lesions. The primary cancer cells that have spread to the bones are breast cancer cells, so this is not the same as having cancer that originates in the bone.
Almost 70% of people living with secondary breast cancer will develop bone mets at some point, and it is the most common site of metastasis for breast cancer. People diagnosed with oestrogen receptor positive (ER+) breast cancer are more likely to develop bone mets than other subtypes.
The bones that are most commonly affected are:
- Arms and legs (particularly the upper areas)
- Pelvis
- Ribs
- Skull
- Spine
Common symptoms of bone mets:
- Pain, especially at night
- Bones are weaker, less dense, and more prone to fractures
- Feeling thirsty and unwell due to calcium released into the blood
- Spinal cord compression
If you have any concerns regarding symptoms, you should contact your GP or local medical centre.
Bone mets are typically managed with whole-body treatments that treat cancer cells no matter where they are in the body. This includes options such as hormone therapy, targeted therapy, chemotherapy, and radiotherapy. Symptom management may also include bone-strengthening drugs, surgery, or pain relief.
Treatment Main Purpose Additional Purpose
Research is underway looking into developing new therapies based on nanotechnology that will deliver anti-cancer drugs specifically to the sites of bone mets.
Secondary Breast Cancer in the Brain
When breast cancer cells spread to the brain, it is commonly known as brain metastases, or brain mets. The primary cancer cells that have spread to the brain are breast cancer cells, so this is not the same as having cancer that originates in the brain.
Occasionally, breast cancer cells can spread to the tissues (membranes) that surround the brain and spinal cord. This is known as leptomeningeal metastases.
10-15% of people with secondary breast cancer will get brain metastases. Most of these people won’t get brain mets until after their breast cancer has already spread to other parts of the body. Younger people, especially those under 40 at the time of their breast cancer diagnosis, are at a greater risk of developing brain mets. You are more likely to get brain metastases if you have HER2-positive (HER2+) or triple negative breast cancer (TNBC).
There are a variety of symptoms you may experience, depending on what part of the brain is affected. Common symptoms of brain mets include:
- Headaches that are not relieved with pain medication
- Changes in personality, mood, or behaviour
- Confusion
- Dizziness or loss of balance
- A feeling of weakness or numbness on one side of your body
- Seizures (fits)
- Memory loss
- Changes in vision
- Nausea and/or being sick
- Speech difficulties
 If you have any concerns regarding symptoms, you should contact your GP or local medical centre.
If you have any concerns regarding symptoms, you should contact your GP or local medical centre.
Brain mets are typically managed with whole-body treatments that treat cancer cells no matter where they are in the body, such as hormone therapy, targeted therapy, immunotherapy or chemotherapy. A challenge in treating secondary breast cancer in the brain is that the brain is surrounded by a barrier that prevents many substances (including many cancer drugs) from entering the brain. This is known as the blood-brain barrier. This means that some drug treatments that can kill cancer cells in other areas of your body are unable to reach the cancer cells in your brain.
More targeted treatments such as steroids, radiotherapy, and anticonvulsants can help slow the growth of brain mets and relieve symptoms. Surgery may also be an option. Other targeted therapy options include the CyberKnife and Gamma Knife (see the video in the Secondary Breast Cancer of the lungs section). These are machines that can deliver radiotherapy with pinpoint accuracy. They are available at some cancer centres. You can discuss with your clinical team about which treatment options are suitable for you.
 Research has shown that diagnosing brain mets before symptoms develop can lead to better overall survival. Make 2nds Count is funding a study that explores Magnetic Resonance Imaging (MRI) monitoring as a tool for early detection of brain mets. This is called the HER2-CNS SURVEILLANCE Study, and is due to start recruiting secondary breast cancer patients in 2024.
Research has shown that diagnosing brain mets before symptoms develop can lead to better overall survival. Make 2nds Count is funding a study that explores Magnetic Resonance Imaging (MRI) monitoring as a tool for early detection of brain mets. This is called the HER2-CNS SURVEILLANCE Study, and is due to start recruiting secondary breast cancer patients in 2024.
Make 2nds Count is also supporting the PRIMROSE Studies that will study cerebrospinal fluid (CSF) and tissue to understand more about cancer cells that spread to the brain. Greater understanding about these cancer cells can help us better understand treatment options.
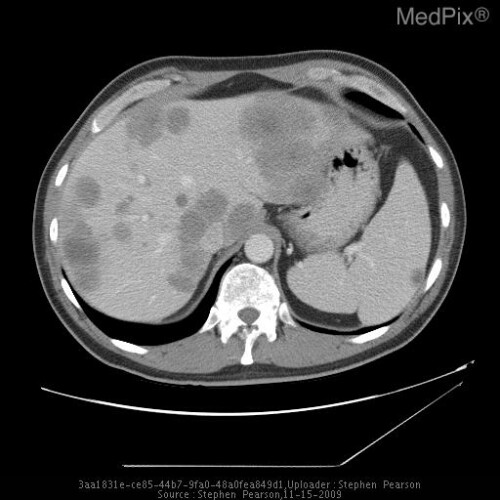
Secondary Breast Cancer in the Liver
When breast cancer cells spread to the liver, it is commonly referred to as liver metastases, or liver mets. The primary cancer cells that have spread to the liver are breast cancer cells, so this is not the same as having cancer that originates in the liver.
About half of people diagnosed with secondary breast cancer develop liver mets. People who have liver mets often have metastasis in other parts of their body as well, but not always.
 It can be difficult to diagnose liver mets because most of the time it does not cause new symptoms unless liver function is being affected. Possible symptoms include:
It can be difficult to diagnose liver mets because most of the time it does not cause new symptoms unless liver function is being affected. Possible symptoms include:
- Ascites (swelling in your stomach area)
- Pain or discomfort on the right side of the stomach, under the ribs. This may radiate to the right shoulder
- Jaundice (the skin and whites of the eyes appear yellow)
- Feeling itchy
- Hiccups
- Generally feeling unwell
If you have any concerns regarding symptoms, you should contact your GP or clinical team.
Liver mets are typically managed with whole-body treatments that treat cancer cells no matter where they are in the body, such as hormone therapy, targeted therapy, or chemotherapy. However the liver is difficult to treat because its function is to break down toxins and drugs (such as your cancer treatments) rather than let them do their job.
More targeted options may include surgery, or less invasive treatments like radiotherapy, ablation (applying heat, cold, or alcohol directly to the tumour), or embolization (blocking blood flow to the tumour so that the tumour cells cannot survive). Talk to your clinical team about the most suitable options for you.
Future treatments are likely to borrow from the research already done on liver metastasis in colorectal cancer. This should give us new options for specific drugs, drug delivery methods and surgery.
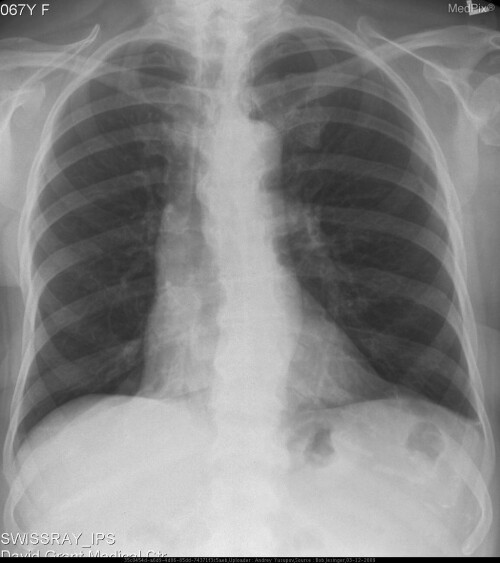
Secondary Breast Cancer in the Lungs
When breast cancer cells spread to the lung, it is commonly referred to as lung metastases, or lung mets. Breast cancer cells travel through the bloodstream or lymphtatic system to the lung, so occasionally, the lymph nodes within the middle of the chest can also be affected. The primary cancer cells that have spread to the lung are breast cancer cells, so this is not the same as having cancer that originated in the lung.
The lungs are the second most common place for breast cancer to spread, after bones. People diagnosed with triple negative breast cancer (TNBC) are more likely to develop lung mets than people with other breast cancer subtypes, but lung metastasis can happen in anyone.
 Common symptoms of lung mets:
Common symptoms of lung mets:
- A constant cough that will not go away
- A feeling of tightness or pain in your chest that will not go away
- Feeling breathless
Symptoms range from fairly mild to severe, depending on where in the lung the cancer has spread to, and whether both lungs are affected.
If you have any concerns regarding symptoms, you should contact your GP or clinical team.
Lung mets and their symptoms are typically managed with whole-body treatments that treat cancer cells no matter where they are in the body. This includes hormone therapy, targeted therapy, or chemotherapy. Treatments may also include surgery or radiotherapy.
The CyberKnife is a machine that can deliver radiotherapy with pinpoint accuracy. It is available at some cancer centres. You can discuss with your clinical team whether CyberKnife is a suitable treatment option for you.
Lots of research is underway looking at the molecular pathways that drive lung metastasis. This gives us hope for the future that new targeted drugs can be found to block these pathways, especially for the TNBC subtype where fewer treatment options are available.
Secondary Breast Cancer in the Skin
When breast cancer cells spread to the skin, it is commonly referred to as skin metastases, skin mets, or lesions. They may form on or just below the skin. The primary cancer cells that have spread to the skin are breast cancer cells, so this is not the same as having cancer that originates in the skin. Skin metastases can also be known as cutaneous metastasis.
Around one third of people with secondary breast cancer will develop skin mets. The most common places on your body to get skin mets are near the site of the breast cancer, such as on the chest, around a surgical scar, or on the abdomen (belly).
Skin mets can occur (less commonly) on other skin areas, for example on the arms, back, neck and scalp.
Common symptoms of skin mets include:
- Change in skin colour
- Persistent rash, including redness and inflammation
- One small firm lump (nodule) or multiple lumps of different sizes
- Swelling of the area, known as lymphoedema
- Pain
- Bleeding
- Infection
- Smell
There is a lack of information about detecting secondary breast cancer of the skin in people of colour. If you have any concerns regarding symptoms, you should contact your GP or local medical centre.
Symptoms of skin mets can be managed with pain relief and antibiotics. More targeted therapies can include radiotherapy, chemotherapy, specialist dressings, surgery and electrochemotherapy (ECT). ECT is a relatively new treatment that combines a low dose of chemotherapy drug with small electrical impulses. It can help to minimise bleeding, broken skin, pain and reduce the size of the skin mets. Discuss with your clinical team about which treatment options are suitable for you.
Another type of therapy, known as Photodynamic Therapy (PDT) has shown benefits in the treatment of non-melanoma skin cancers, such as in secondary breast cancer of the skin. For this treatment, a drug is applied to the metastasis that makes the cancer cells sensitive to a particular type of light. Doctors then shine this bright light on the treatment area and the drug reacts with the light to destroy the cancer cells.
Current research aims to gain a better understanding of these various treatment options for skin metastasis and this will help us learn what are the best options for patients.
Below are some images of skin mets from secondary breast cancer patients.
Less Common Sites of Secondary Breast Cancer
The bones, lungs, liver, brain, and skin are the most common places for secondary breast cancer to spread to in the body. However, sites of metastasis can be anywhere in the body. Less common sites include lymph nodes, soft tissues, endocrine glands, eyes, mouth, ears, nose, reproductive organs, heart, stomach, colon, pancreas, meninges (membranes that surround your brain and spinal cord) and more. Your healthcare team will be able to give you more specific information if your secondary breast cancer is in one of these less common sites.
At Make 2nds Count, our priority is to support people with secondary breast cancer diagnoses and their families, and to empower them with knowledge about their condition. If you want to learn more about specific treatments for secondary breast cancer, you can read our webpage dedicated to Treatments.
Written by Clare McDonald, University of Edinburgh
Reviewed by Dr Sarah Thomas and Dr Alexander Kolliari-Turner, Make 2nds Count
Date of last update: May 2024




