Understanding Your Diagnosis
A secondary breast cancer diagnosis can have lots of medical terms that you might not be familiar with and can be difficult to understand at first. This educational page provides some basic information about how secondary breast cancer is diagnosed and the different subtypes of secondary breast cancer to help you understand your diagnosis. These classifications are important because they determine what treatment options will be available to you.
On this page, you will find:
How is Secondary Breast Cancer Diagnosed
The main way secondary breast cancer is diagnosed is via the use of imaging and/or biopsies.
Imaging
Imaging is a medical technique which tests to see if the cancer has spread. The most common imaging techniques include X-Rays, Ultrasounds and MRI Scans. These tests are helpful for your clinical team to understand how far and where the cancer has spread. This can help identify the best treatments and provide more information about your symptoms.
For more information on imaging visit the types of scans page.
Biopsies
A biopsy is when a small sample of tissue is taken from the secondary tumour and looked at under a microscope. A tumour biopsy helps your care team to understand characteristics of the secondary breast cancer.
Why do I need a biopsy?
In secondary breast cancer, tumour biopsies are done to check if the features of the cancer have changed since the primary diagnosis. For example, the types of receptors present on the surface of the secondary breast cancer cells might be different to the primary diagnosis. This is important information as treatment decisions based on the receptors of the primary breast cancer may not always be suitable for the treatment of the secondary breast cancer.
Further down this page you can learn more about the main subtypes of secondary breast cancer and the receptors used to classify these subtypes.
Biopsy samples are looked at under the microscope to generate a pathology report. Owise's blog; ‘Your Pathology Results Explained’ can help you better understand the pathology results from a biopsy.
Tissue Biopsy (sometimes referred to as Needle Biopsy)
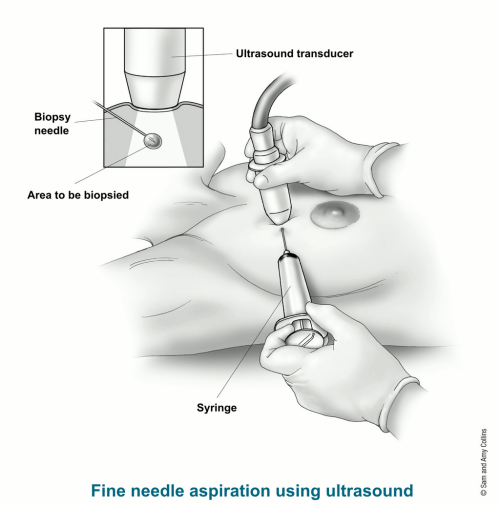 A tissue biopsy is when a small sample of tissue is taken from the secondary tumour and looked at under the microscope. This can be taken from many parts of the body, including lymph nodes, lungs, liver, bone and skin. Tissue biopsies are done using a needle which is inserted through the skin and into the part of the body being examined. This needle will then cut out a very small sample of tissue. During this process, local anaesthetic is used to minimise any pain or discomfort. The area may bleed a little after the biopsy, so you will usually be provided with a small plaster or dress.
A tissue biopsy is when a small sample of tissue is taken from the secondary tumour and looked at under the microscope. This can be taken from many parts of the body, including lymph nodes, lungs, liver, bone and skin. Tissue biopsies are done using a needle which is inserted through the skin and into the part of the body being examined. This needle will then cut out a very small sample of tissue. During this process, local anaesthetic is used to minimise any pain or discomfort. The area may bleed a little after the biopsy, so you will usually be provided with a small plaster or dress.
The Main Subtypes and Why They Matter
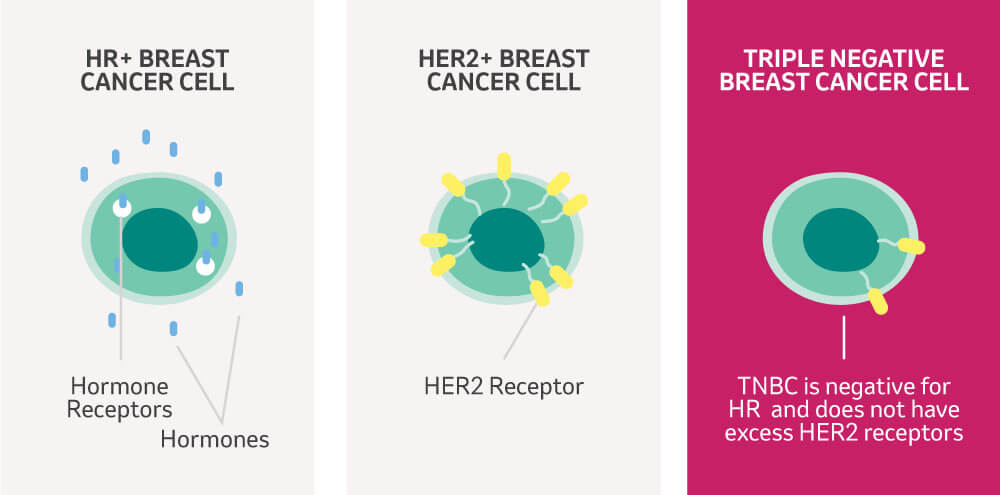
Breast cancers are divided into different categories based on the presence or absence of certain receptors on the cell surface. Receptors act like docking stations for specific molecules, such as hormones and growth factors, which can stimulate cancer growth. Therefore, many breast cancer treatments will target these receptors or the molecules that bind to them. The different breast cancer categories are also known as molecular subtypes.
The main subtypes are based on the presence or absence of the hormone receptors (HR) oestrogen (ER) and progesterone (PR) and human epidermal growth factor receptor 2 (HER2). If none of these receptors are present your subtype would be known as Triple Negative breast cancer (TNBC). 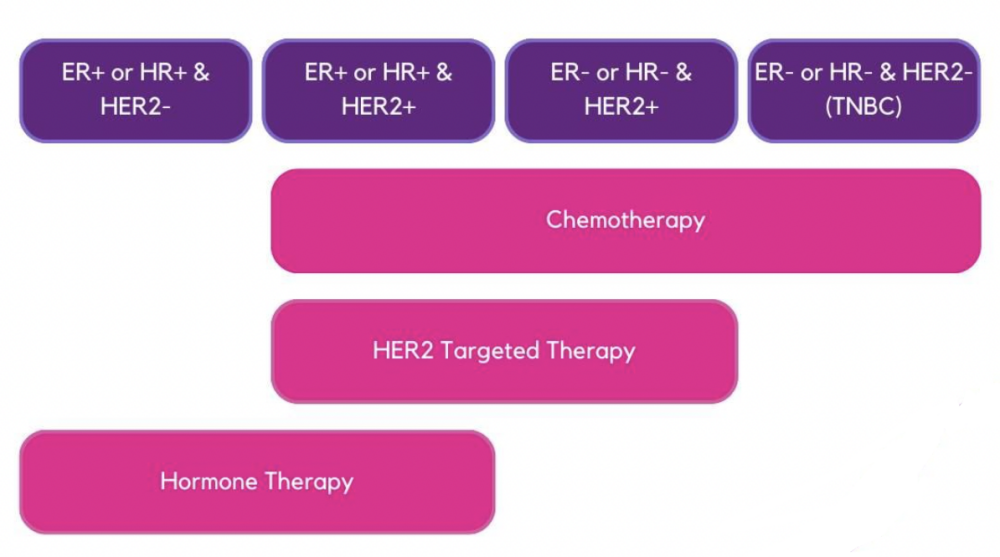
Identifying the subtype of breast cancer is helpful for several reasons:
-
Targeted Treatment: Knowing the subtype helps oncologists determine treatments that can directly target the receptors, hormones or factors that are associated with growth of those cancer cells. For example, HR+ cancers may be treated with hormone therapies that block oestrogen or progesterone from fueling cancer growth, while HER2+ cancers may respond well to drugs that target the HER2 receptor.
-
Access to New Treatments: Clinical trials investigate new treatment options and your subtype can determine if you will be eligible to receive these treatments. You can learn more about clinical trials by speaking to Research Nurses via our Patient Trials Advocate service.
-
Informed Decisions: Understanding your cancer type can empower you with knowledge. It helps you know what treatment options to expect and take part in shared decision making about your treatment plan.
-
Prognosis and Outcome: The subtype of secondary breast cancer can give some clues about potential further growth and spread of the disease. This helps in planning your treatment and follow-up care.
Hormone Receptor Status
What Does Hormone Receptor-Positive and Negative Mean?
Some breast cancer cells grow faster when they come into contact with the body's natural hormones, primarily oestrogen and progesterone. These hormones can attach to their specific receptors and help the cancer to grow (Figure 1). This interaction is a key driver in the progression of hormone receptor-positive (HR+) cancers.
-
ER+ (Oestrogen Receptor-Positive): If your cancer is ER+, it means these cancer cells have receptors that attach to oestrogen and oestrogen can make the cancer cells grow faster.
-
PR+ (Progesterone Receptor-Positive): If your cancer is PR+, it means these cancer cells have receptors that attach to progesterone and progesterone can make the cancer cells grow faster.
-
Conversely, if your cancer lacks these receptors, it is classified as Hormone Receptor-negative (HR-) and it doesn't grow due to the presence of these hormones.
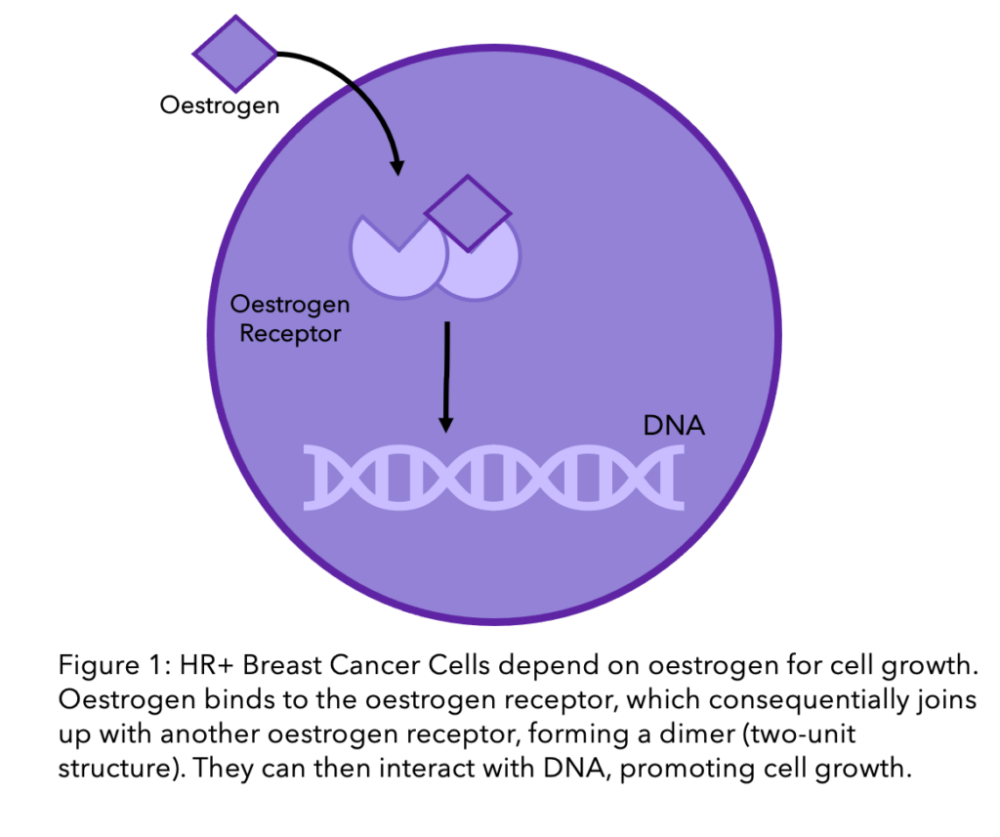
Treatment Options
For HR+ cancers, oncologists often use hormone-blocking treatments. These can stop the hormones from reaching the cancer cells or lower the amount of hormones in the body, slowing down HR+ cancer growth. Treatments can vary if you are pre or postmenopausal because after the menopause the level of hormone production in the body changes. For younger women, some hormone treatments might cause menopause to start earlier, which is an important side effect to consider. You can learn more about different hormone treatment options by clicking here and the menopause and secondary breast cancer by clicking here.
For HR- cancers, these hormone-blocking treatments aren't effective. Instead, doctors might suggest chemotherapy or other treatments that target the cancer cells in different ways.
HER2 Status
What Does HER2-Positive and HER2-Negative Mean?
HER2-positive means you have higher levels of the HER2 receptor on the surface of the cancer cells (Figure 1). These high levels of HER2 receptors are associated with cancer cell growth. Many treatments exist that target the HER2 receptor. However, if your cancer cells do not express the HER2 receptor, you will be classified as being HER2-negative. HER2 specific treatments won't be effective and your medical team will recommend alternative strategies. You can learn more about HER2+ secondary breast cancer by reading this article. 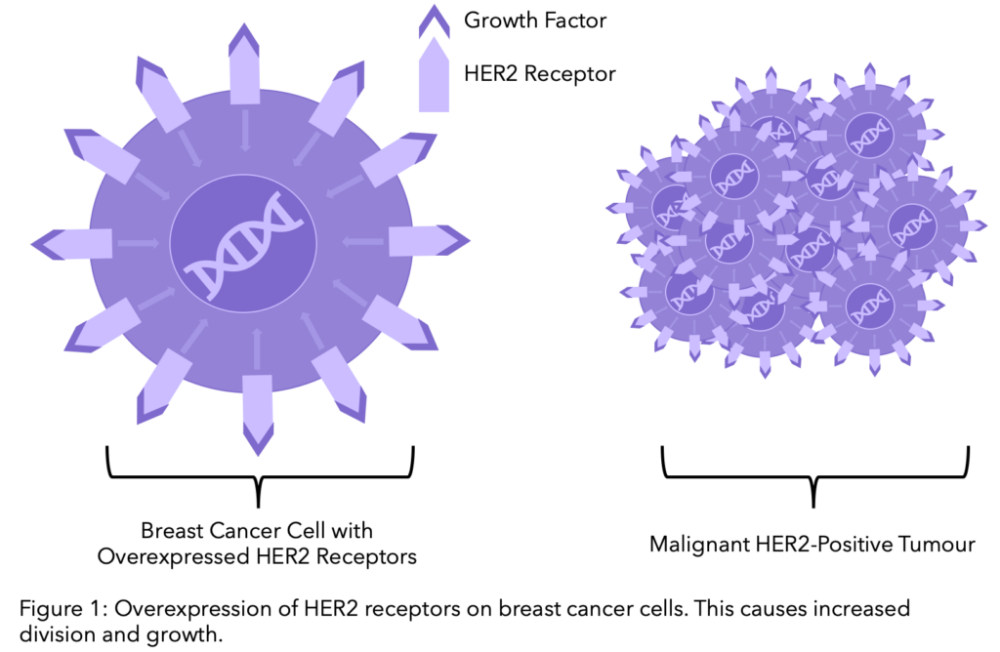
Being “HER2-low” refers to cancers that have lower levels of HER2 protein—not enough to be considered HER2-positive but more than those considered HER2-negative—representing a distinct category that may benefit from emerging treatments designed to target this intermediate level of HER2 expression. Approximately 15% of breast cancers are HER2+, 45-55% are HER2-low and 30-40% are HER2-. You can learn more about HER2-low secondary breast cancer by reading this article.
Treatment Options
Knowing whether your cancer is HER2-positive or negative is vital because it directly influences your treatment options. HER2-positive cancers may be treated with targeted therapies such as Trastuzumab (Herceptin®) or Trastuzumab emtansine (KADCYLA®), which specifically target the HER2 receptor. These therapies can block the signals that tell cancer cells to grow or deliver chemotherapy directly to the cancer cells, providing a more targeted approach with potentially fewer side effects. You can learn more about secondary breast cancer treatment options by clicking here.
It's also important to note the HER2 status of a cancer can change, particularly when it spreads or in response to treatment. The HER2 status of secondary tumours can be tested to ensure that your treatment plan remains aligned with the current characteristics of your cancer.
TNBC (Triple Negative Breast Cancer)
Triple Negative Breast Cancer (TNBC) is characterized by cancer cells lacking the three commonly tested receptors—oestrogen (ER), progesterone (PR), and human epidermal growth factor 2 (HER2). This means that the growth of these cancer cells is not fueled by any of these hormones or growth factors. Therefore, treatments that target these hormones or receptors won't work for TNBC.
TNBC accounts for ~15% of all breast cancer cases and around 8,000 women are diagnosed with TNBC in the UK each year. TNBC is harder to treat than other breast cancer types, has a higher risk of spreading and disproportionately affects women under 40 and those from black backgrounds.
Treatment Options
Since TNBC doesn't respond to hormonal therapy or HER2-targeted treatments, it's often treated with medicines that target other markers, or chemotherapy. For example, a secondary TNBC tumour can be tested for a protein that is found on the surface of cancer cells known as PD-L1 (anti-programmed cell death-ligand 1). If PD-L1 positive, a patient could be offered an immunotherapy treatment such as Atezolizumab (Tecentriq®) or Pembrolizumab (KEYTRUDA®) in combination with chemotherapy. Immunotherapy is a type of targeted biological therapy that helps the immune system to recognise and attack cancer cells.
After two or more treatment lines, Sacituzumab govitecan (Trodelvy®) could be used to treat secondary TNBC and this targets the TROP-2 receptor.
You can learn more about the different treatment options for TNBC by reading this article.
How We Can Help
Being diagnosed with secondary breast cancer can feel like an insurmountable challenge, but you don't have to face it alone. There are numerous support services and resources available to help guide you through this difficult time, providing not only practical information but also emotional support for both you and your loved ones.
At Make 2nds Count, we are here for you.
We offer:
-
Online yoga sessions tailored to those living with secondary breast cancer
-
Online mindfulness sessions to promote mental and emotional health
-
Online breathwork sessions to ease stress, anxiety, pain and tension
There are lots of local support services available for people living with secondary breast cancer, but it’s not easy to find them! Check out our 2nds Support Hub to see what’s available near you.
Written by Yuchen Nie, University of Edinburgh
Reviewed by Dr Alexander Kollari-Turner, Make 2nds Count
Date of last update: May 2024
