Side Effects and Secondary Breast Cancer
It is normal for individuals living with secondary breast cancer to experience a variety of side effects. The side effects you experience will vary depending on where the cancer has spread to in your body and the type of treatment you are on. As side effects are very common and can have a large impact on day-to-day life, there is a lot of support to help you and your loved ones manage them. You can find information about common side effects, how best to manage them and the support Make 2nds Count provides on this page.
On this page you will find:
Common Side Effects; What they are, why they happen and how to manage them:
How we can help
Fatigue
What is fatigue?
F atigue is tiredness which does not go away with rest. Fatigue can affect a person physically and psychologically and limit them from doing day to day activities.
atigue is tiredness which does not go away with rest. Fatigue can affect a person physically and psychologically and limit them from doing day to day activities.
What causes fatigue?
Fatigue is very common amongst individuals living with secondary breast cancer and it can be caused by a variety of reasons. The most common reason is because of the effects of the disease itself. Fatigue may be related to treatments such as chemotherapy, hormone treatment, radiotherapy or surgery, or medicines, such as strong pain relief and anti-sickness tablets. Some patients can also experience fatigue because of emotional stress.
How best to manage fatigue?
If you are experiencing fatigue, it is recommended to speak to your oncologist or GP about your symptoms as underlying causes may be identified. For example, the fatigue could be because of low red blood cells (anaemia) from chemotherapy or endocrine treatment and this can often be easily corrected.
Although it can sometimes be hard to treat the cause of cancer fatigue, there are a number of lifestyle changes that could alleviate symptoms. For example, it is recommended to drink sufficient amounts of water, eat a healthy and balanced diet, exercise regularly, accept help with day-to-day tasks and maintain a regular sleep schedule.
Feeling Sick/Nausea
What is nausea?
Nausea  is feeling the urge to vomit. You may experience an uncomfortable feeling in the back of your throat or your stomach. It can also make you feel lightheaded and dizzy. It is important to recognise that nausea does not always lead to vomiting, but it can make day-to-day life more difficult.
is feeling the urge to vomit. You may experience an uncomfortable feeling in the back of your throat or your stomach. It can also make you feel lightheaded and dizzy. It is important to recognise that nausea does not always lead to vomiting, but it can make day-to-day life more difficult.
What causes nausea?
There are many reasons you may feel nauseous. It may be caused by the disease, treatments, such as chemotherapy drugs, targeted cancer drugs, immunotherapy and hormone therapies. Some patients also experience nausea because of anxiety surrounding their diagnosis.
How best to manage nausea?
If you are experiencing sickness/nausea, you should speak to your oncologist or GP as they will be able to prescribe anti sickness drugs (antiemetics). They will advise you to take these anti sickness drugs regularly, whether you feel sick or not. This is because these drugs are much better at preventing sickness than stopping it once it starts.
Other methods are available to complement anti sickness drugs. These include exercise, muscle relaxation training, cognitive behavioural therapy (CBT) and activities that can provide a distraction (e.g., listening to music or playing video games). If you are nauseous or sick after chemotherapy you might want to try having a small meal a few hours before chemotherapy, not just before.
Bone Pain
What is bone pain?
Bone  pain is any pain or discomfort you feel in your bones and joints. It typically gets worse at night.
pain is any pain or discomfort you feel in your bones and joints. It typically gets worse at night.
What causes bone pain?
If someone living with secondary breast cancer experiences bone pain, there is a possibility this is happening because the cancer has spread to the bones. This is known as bone metastasis or bone mets. The bones most commonly affected are the spine, ribs, skull, pelvis and upper bones of the arms and legs. If this happens, your bones will become weaker and they are more likely to break.
Bone mets can cause spinal cord compression (causing back pain) and can lower blood cell count, increasing the risk of infection, anaemia, bruising and bleeding. Advanced bone mets can cause calcium to go into the bloodstream, causing too much calcium in the blood (hypercalcaemia). Symptoms of hypercalcaemia include passing lots of urine, feeling thirsty and fatigue.
How best to manage bone pain?
If you are experiencing bone pain, you should speak to your oncologist or GP. They might recommend you have further scans to investigate if the cancer has spread to your bones and they can prescribe pain relief medications. They can also prescribe bone strengthening medications, known as bisphosphonates which can help strengthen the bones by reducing destruction of bones by the disease and stop hypercalcaemia effects.
Breathlessness
What is breathlessness?
Breathlessness  is also known as shortness of breath.
is also known as shortness of breath.
What causes breathlessness?
If you have severe difficulty breathing (e.g., you’re gasping, choking or not able to get words out), alongside chest pains or have pain that spreads to your arms, back, neck or jaw you should call 999 or go to A&E immediately. This could be a sign of pulmonary embolism, heart failure or stroke.
Shortness of breath can also slowly present itself over time. If you start to experience breathlessness after normal activities, when you lie down, or have a persistent cough you should mention this to your oncologist or GP. Breathlessness can be caused by being overweight, having asthma or a chest infection, but it can also be a sign that breast cancer might have spread to the lungs. You should not try to self-diagnose the cause of your shortness of breath. Your oncologist or GP may advise you to have further scans to investigate if the breast cancer has spread to your lungs.
How best to manage breathlessness?
If you are experiencing breathlessness due to disease causing fluid to build up in the lungs, you may have to get the fluid drained from your lungs. You may also be recommended for a treatment called pleurodesis. This treatment seals the two layers of the pleura together. This is a minor surgery, and you will need to stay in hospital for a few days.
Constipation
What is constipation?
Constipation  is where you have changes to how you poo, including not pooing as often or finding it hard to poo.
is where you have changes to how you poo, including not pooing as often or finding it hard to poo.
What causes constipation?
Constipation can be caused by cancer treatment. Some chemotherapy medicines can cause constipation because they affect the nerve supply to the gut. Other medicines used to manage secondary breast cancer, such as painkillers, anti sickness drugs and bone strengthening drugs (bisphosphonates) can also cause constipation. Combinations of these drugs can also worsen the level of constipation that patients experience.
How best to manage constipation?
Constipation can be difficult to talk about, but it is recommended that you discuss this with your oncologist or GP as they could prescribe a laxative. They might also recommend that you make some changes to your diet, such as slowly increasing fibre intake by eating more fresh fruit and vegetables, drinking more water, avoiding alcohol and increasing your level of daily activity.
Lymphoedema (swelling of the arm or leg)
What is Lymphoedema?
L ymph fluid is present in all body tissues and usually drains into the bloodstream through channels called lymph vessels that are part of the lymphatic system. However, if the lymph drainage channels or lymph nodes are blocked, damaged or removed lymph fluid can build up and cause swelling, which is known as lymphoedema. Lymphoedema is a chronic condition that mostly affects the arms or legs, but it can also affect other parts of the body. It cannot be cured but treatments are available to help control it.
ymph fluid is present in all body tissues and usually drains into the bloodstream through channels called lymph vessels that are part of the lymphatic system. However, if the lymph drainage channels or lymph nodes are blocked, damaged or removed lymph fluid can build up and cause swelling, which is known as lymphoedema. Lymphoedema is a chronic condition that mostly affects the arms or legs, but it can also affect other parts of the body. It cannot be cured but treatments are available to help control it.
What causes Lymphoedema?
Lymphoedema can be caused by cancer that blocks a lymph node or lymph vessels. Surgery to remove lymph nodes can also cause lymphoedema, as can damage to the lymph nodes from cancer treatments such as radiotherapy. Not everyone who has cancer or cancer treatment will develop lymphoedema and more research is needed to work out how many people will develop lymphoedema.
How best to manage Lymphoedema?
If you are experiencing Lymphoedema you should contact your oncologist or GP. Lymphoedema treatments help to reduce fluid build up and encourage the flow of fluid through the lymphatic system to control and reduce the swelling where possible. The main treatments include compression therapy and manual lymphatic drainage. You will also be advised to maintain good skin hygiene in the swollen area, as keeping the skin dry and moisturised can prevent injury and infection. Exercise can also help to keep lymph fluid flowing through the lymphatic system and help you maintain a healthy weight.
Early Menopause
What is early menopause?
This is when an individual experiences menopause earlier than their biological clock. Common symptoms include hot flushes, night sweats, difficulty sleeping, mood fluctuations and problems with concentration.
What causes early menopause?
Early menopause happens because the ovaries, which produce oestrogen, can be affected by the treatment you are on, and stop producing eggs prematurely. Treatments such as chemotherapy and hormone therapy are the main reasons why you can experience an early menopause or symptoms of menopause.
How best to manage menopause?
Menopause symptoms from cancer treatment can be sudden and intense. If you are having a difficult time coping with symptoms you should speak to your oncologist or GP as a number of different options are available for symptom management. Visit our information page on the menopause to learn more. 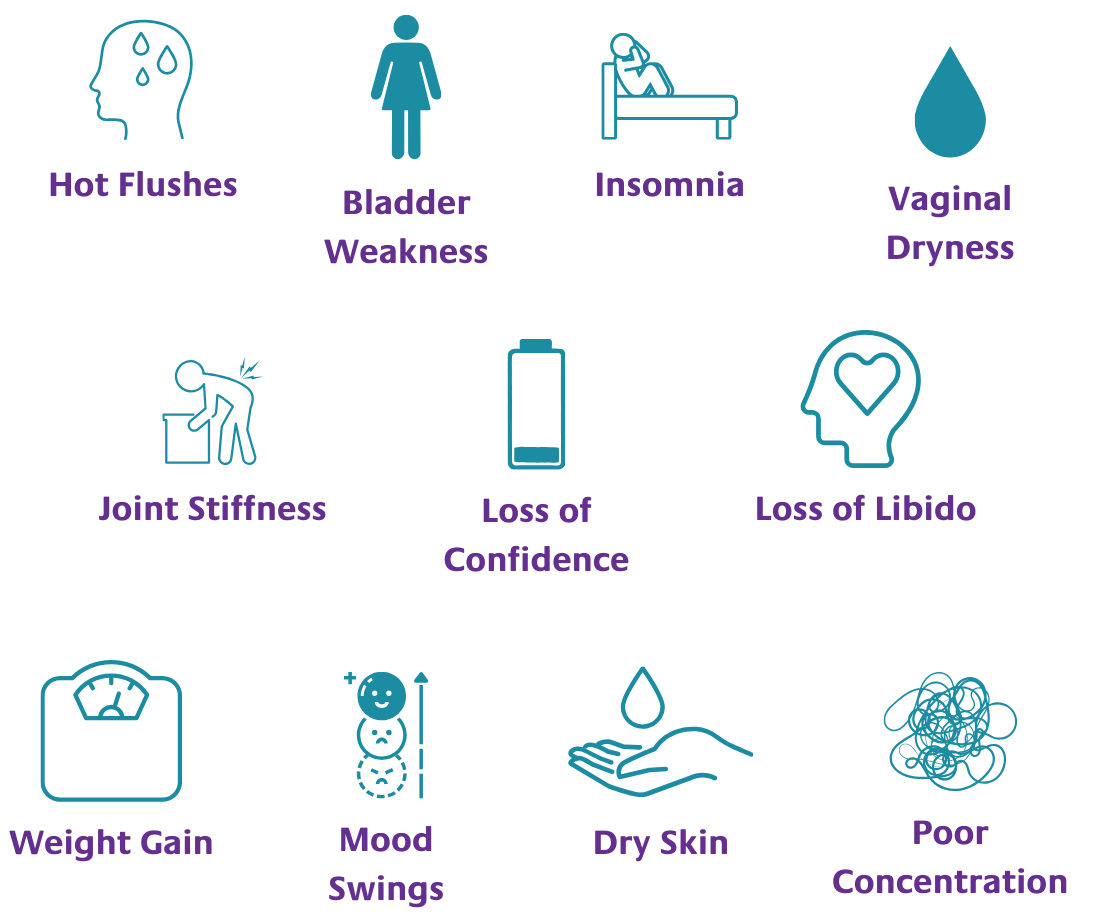
Insomnia
What is insomnia?
Insomnia is when someone has difficulty falling asleep at night, staying asleep at night and waking up too early in the morning.
 What causes insomnia?
What causes insomnia?
Insomnia can be caused by lots of different reasons when you have cancer, these include:
-
Cancer related symptoms (such as pain and nausea)
-
Side effects of treatment
-
Worry, anxiety or depression
How best to manage Insomnia?
If your insomnia is being caused by cancer related symptoms, such as pain or nausea, it’s important to tell your oncologist or GP as they might be able to prescribe medications, such as painkillers or anti-sickness medicines that can help. Some treatments, such as corticosteroids (anti-inflammatory steroids) can make it difficult to fall asleep if taken at night time, so you could discuss with your clinical team if you could take them in the morning instead.
Some anti sickness medicines make patients feel restless, if this happens talk to your doctor and they might be able to prescribe a different type.
There are a number of lifestyle habits that can also improve your sleep, such as:
-
Avoid caffeinated drinks 6 hours before you go to bed
-
Avoid eating a large meal 2 hours before bedtime
-
Having a regular bedtime routine
-
Trying to have some physical activity during the day
-
Avoid checking or watching the clock during the night
-
Try and avoid napping during the day
-
Minimising noise and light in the bedroom
-
Keeping a temperature in the bedroom that is not too hot or cold
You can learn more about managing insomnia whilst having cancer by reading this article.
Fear and Anxiety
What is fear and anxiety?
Anxi ety is a feeling of unease, such as worry or fear, that can be mild or severe.
ety is a feeling of unease, such as worry or fear, that can be mild or severe.
What causes fear and anxiety?
Patients living with secondary breast cancer can experience fear and anxiety due to uncertainty around their diagnosis. This is a common and normal feeling.
How best to manage fear and anxiety?
A lot of support exists to help manage fear and anxiety over the future. Talking to others and joining an online or in-person support group can help manage these feelings. You should speak to your oncologist or GP if you are experiencing persistent anxiety as they may prescribe anti-anxiety medications as part of your treatment.
Side Effects of Chemotherapy/Radiotherapy
What are the common side effects?
Che motherapy and radiotherapy can cause several side effects, some of which have been mentioned above. However, they can also cause a number of other side effects. The side effects you experience will depend on where you are receiving radiotherapy and the type of chemotherapy. Common side effects include:
motherapy and radiotherapy can cause several side effects, some of which have been mentioned above. However, they can also cause a number of other side effects. The side effects you experience will depend on where you are receiving radiotherapy and the type of chemotherapy. Common side effects include:
-
General pain in the treatment area
-
Changes to skin in the treatment area – irritation, itchiness, dryness, redness, swelling and a change in colour
-
Swelling of the breast
-
Changes in shape, size and feel of breast
-
Hair loss
-
Stiffness in the arm and shoulder
-
Kidney and bladder problems
-
Loss of appetite
-
Trouble remembering and concentrating - sometimes known as “chemo brain”
What causes these side effects?
The side effects from chemotherapy and radiotherapy occur because in the process of damaging cancer cells these treatments can also damage healthy cells.
How best to manage these side effects?
Numerous treatments are available to manage the side effects from chemotherapy and radiotherapy. Click here for more information on chemotherapy side effects and click here for more information on radiotherapy side effects.
How we can help
Coping with secondary breast cancer and the side effects of treatment can be challenging. At Make 2nds Count, we are here for you.
We offer:
-
Online yoga sessions tailored to those living with secondary breast cancer
-
Online mindfulness sessions to promote mental and emotional health
-
Online breathwork sessions to ease stress, anxiety, pain and tension
There are lots of local support services available for people living with secondary breast cancer but sometimes it’s not easy to find them! Check out our 2nds Support Hub to see what’s available near you or speak to your Breast Nurse Specialist or treatment team to get more information.
Written by Emily Foster, University of Edinburgh
Reviewed by Dr Alexander Kolliari-Turner, Make 2nds Count & Pauline McIlroy, retired Advanced Breast Clinical Nurse Specialist in Oncology from the Beatson West of Scotland Cancer Centre
Date of last update: June 2024
