3rd March 2021 Education

In the first blog of our series in partnership with Make 2nds Count, we want to share with you reliable information surrounding secondary breast cancer and the available treatments. Nearly a third of people diagnosed with earlier stages of breast cancer will eventually develop advanced disease [1, 2]. Even though many people are living with secondary breast cancer, it can often feel that it is excluded from breast cancer campaigns. Research has shown that women with advanced breast cancer often feel isolated and 67% of them feel like no one understands what they are going through [3,4].
In this blog, we will be sharing with you accessible treatments for advanced hormone receptor positive, HER2 negative breast cancer (if you are HER2 positive, head to our previous blog).
What is hormone positive HER2 negative advanced breast cancer?
Secondary breast cancer (also called metastatic, advanced, or stage IV) is a breast cancer that has spread beyond the breast and nearby lymph nodes to other parts of the body. Hormone receptor positive (ER positive) HER2 negative advanced breast cancer indicates that cancer cells grow in response to the hormones oestrogen and progesterone but not in response to the protein HER2.
Although it is possible to be initially diagnosed with secondary breast cancer (called “de novo metastasis”), it is more common to develop metastatic disease after being previously treated for a localised breast cancer. In fact, a study that looked back at 60,000 women with ER positive localised breast cancer after hormone therapy showed that even some patients with low risk breast cancer (<2 cm tumours, lymph node negative) develop metastatic cancer [5]. Women that finish hormone therapy five years after having surgery still have a risk of cancer coming back. Therefore, in order to reduce this probability and increase survival, understanding drug resistance and managing side effects so patients can continue treatment is key.
“Something to look forward to is what everyone does. You might have to scale it back from not looking forward to something that is in five years time, but if you can look forward to something that is in three weeks and something that is in three months, and dare to plan it and dare to believe you be able to enjoy it and you will, you will be able to” [6] (Diane, secondary breast cancer patient)
Your treatment options
We have pulled together all the different treatment options for ER positive, HER2 negative metastatic breast cancer that are available on the NHS. We have classified them into four types: hormone therapy, CDK4/6 inhibitors, PIK3/mTOR inhibitors and chemotherapy. In this blog, we are going to identify them all, explain how each work and whether or not they have been approved by the National Institute for Health and Care Excellence (NICE), or by its Scottish counterpart (SIGN). If you have locally advanced breast cancer (stage III) where the cancer has spread to the surrounding skin, lymph nodes or chest wall, these treatments will also be available to you.
1.Hormone therapy
The goal of hormone therapy in this type of cancer is to decrease oestrogen production and/or activity by breaking the pathway by which oestrogen is produced and interacts with breast cancer cells. In fact, these therapies can control secondary breast cancer for long periods of time and they are usually the treatment offered as first line therapy.
First line therapy refers to the first treatment given for a disease. If this doesn’t cure the disease or causes severe side effects, then second line therapy would be given, and so forth.
a. Ovarian suppression
Ovarian suppression is a first line therapy. Decreasing or stopping ovarian oestrogen production with drugs, such as goserelin (Zoladex®) and Lupron®, or by a surgical removal of the ovaries improves survival [7, 8].
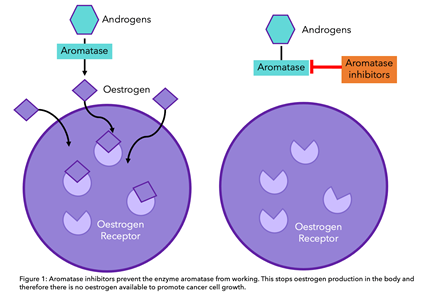
b. Aromatase Inhibitors
Aromatase is a protein that converts androgens (created in the adrenal glands) into oestrogens in the fat, liver, muscle or brain cells. Aromatase inhibitors such as Letrozole (Femara®), Anastrozole (Arimidex®) or Exemestone (Aromasin®) inhibit this conversion, decreasing oestrogen levels in the body. These drugs are used in women who are postmenopausal with secondary breast cancer as they improve progression-free survival compared to other therapies such as tamoxifen [7,9].
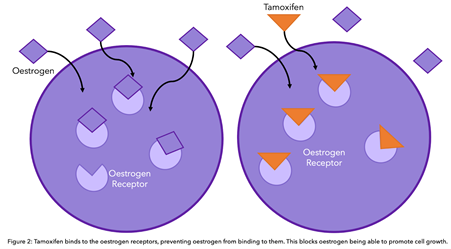
c. Tamoxifen
Tamoxifen binds directly to the oestrogen receptor (ER) of breast cancer cells, reducing oestrogen activity. It is recommended by NICE along with ovarian suppression for men and premenopausal women with advanced disease [10]. To know more about tamoxifen and aromatase inhibitors, head to our previous blog.
d. Fulvestrant
Fulvestrant (Faslodex®) blocks the oestrogen pathway differently to tamoxifen. It binds to the oestrogen receptor (ER) and degrades/breaks this receptor. Therefore, if the oestrogen receptor is degraded, oestrogen cannot bind and drive cancer growth. Fulvestrant is normally offered alongside other therapeutics (find out more below), and is not recommended as an alternative to aromatase inhibitors [11].
4. Why do some patients become resistant to hormone therapy?
Although many people with ER positive breast cancer respond well to hormone therapy, a percentage may become resistant to this treatment after a number of years. Recent studies have looked at the genetics of secondary ER positive tumours and have found some ways by which cancer cells outsmart hormone therapy. In other words, cancer cells change over time and use alternative pathways to grow. This means that they may no longer be dependent on oestrogen (ER negative) and therefore hormone therapies are not effective. To learn more about hormone therapy resistance, head to our previous blog.
5. CDK4/6 inhibitors
CDK4/6 inhibitors are a class of oral drugs that inhibit proteins called CDK4 and CDK6. These proteins are important in cell division.
Cells have a cell cycle which consists of growing, making DNA (genetic material) and then dividing into more cells. This cell cycle is tightly controlled by many proteins, including CDK4 and CDK6. Therefore, if these proteins are blocked, the cell cycle is interrupted and growth and division are stopped [12].
Abemaciclib (Verzenio®), palbociclib (Ibrance®) or ribociclib (Kisqali® ) in combination with an aromatase inhibitor are recommended as a first line treatment by NICE for previously untreated secondary breast cancer [7]. In fact, clinical trials have demonstrated that these treatments improve survival for around 10 months versus using an aromatase inhibitor alone [13, 14, 15, 16]. However, currently there are no biomarkers to predict the response to these therapies [17].
Abemaciclib, palbociclib or ribociclib in combination with fulvestrant can also be prescribed for advanced breast cancer patients treated previously with hormone therapy (second line therapy) under the Cancer Drug Fund, only if Everolimus combined with exemestane (described below) is the only possible alternative [8]. However, very recent NICE draft guidelines now indicate that ribociclib with fulvestrant would be recommended for HR+, HER- locally advanced or secondary breast cancer previously treated with hormone therapy.
What is the Cancer Drug Fund? The Cancer Drugs Fund is part of the British organisation that reviews new and existing drugs, called NICE. It was made to fund new drugs and accelerate the process of drugs becoming available in England. If there are recently developed treatments that may be of benefit to you, your specialist will fill out an application on your behalf. To find out more about Cancer Drugs Fund, head to Cancer Research UK’s website.
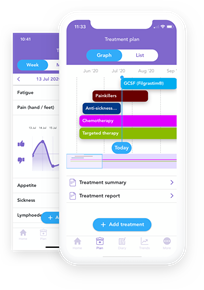
CDK4/6 inhibitors can cause a severe decrease in white blood cells (immune cells). Because of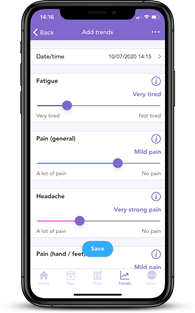 this, palbociclib and ribociclib are followed with a seven-day break to allow white blood cell levels to recover. Abemaciclib can be given continuously however fatigue and diarrhea are often experienced. Liver and heart function tests may also be carried out. [18]. In order to deal with side effects, tracking them through OWise can help evaluate whether a change in CDK4/6 inhibitor may be beneficial.
this, palbociclib and ribociclib are followed with a seven-day break to allow white blood cell levels to recover. Abemaciclib can be given continuously however fatigue and diarrhea are often experienced. Liver and heart function tests may also be carried out. [18]. In order to deal with side effects, tracking them through OWise can help evaluate whether a change in CDK4/6 inhibitor may be beneficial.
6. Everolimus
Everolimus is a targeted therapy that blocks the protein mTOR. This protein affects how cells grow and divide. Everolimus with the aromatase inhibitor exemestane is recommended if other treatments such as hormone therapy are ineffective, due to its success in increasing progression-free survival. As with CDK4/6 inhibitors, there are no biomarkers that predict the response to everolimus, so it cannot be determined prior to treatment if it will be effective for your specific breast cancer [19].
Some of the most common side effects of this therapy are high blood sugar/diabetes, mouth sores, lung inflammation and fatigue. Interestingly, a study found that steroid mouth rinse improves mouth sores from everolimus. Due to its severe side effects, CDK4/6 inhibitors alongside fulvestrant are the preferred treatment [16].
Did you know that Everolimus (Rapamycin) was discovered in Easter Island “Rapa Nui”? [21].
7. Chemotherapy
The most common chemotherapy regimen recommended by the NHS includes both a taxane:
And an anthracycline:
For patients who are not suitable for anthracyclines, docetaxel is offered as first-line treatment, followed by vinorelbine or capecitabine [7].
Gemcitabine can be used when it is combined with paclitaxel, and after other chemotherapy medicines like anthracyclines have either not worked or were considered unsuitable [7].
During the COVID-19 pandemic, chemotherapy regimens have slightly changed. Some common intravenous chemotherapy drugs (e.g Taxol®) are being replaced by oral chemotherapy pills such as Capecitabine (Xeloda®), and Abraxane® might be prioritised over Taxol® due to its reduced toxicity (fewer side effects) (if you want to understand the difference between Taxol and Abraxane, head to this Instagram post). - [22]
a. After chemotherapy: Eribulin
The chemotherapy drug Eribulin is recommended after two or more chemotherapy regimens with anthracycline or taxane, and capecitabine. The most common side effects of this therapy are hair loss, nausea, low white cell counts, fatigue and numbness or tingling [7].
Did you know that eribulin (aka Halaven) was created using a sea sponge?
It's modelled from halichondrin B, which was first discovered in 1986 in marine sponges. Due to its complexity and the lack of it naturally, a synthetic version was made.
8. Metastases
8.1 Bone metastases
If your breast cancer has spread to your bones, there are an array of treatments that you could be offered for both preventing fractures and other bone-related problems, as well as pain management.
a. Bisphosphonates and Denosumab
There are multiple bisphosphonates available, namely zoledronic acid (Zometa®) and ibandronate (Bondronat®), which can be offered either orally or through injections [23].
They act by targeting the cells that break down old bone. In bone metastases, there is already a deficit of healthy bone cells, bisphosphonates prevents bone cell breakdown making the bone denser and less likely to fracture [24].
Denosumab is a type of targeted therapy called a monoclonal antibody. It can be offered instead of bisphosphonates, its function is the same but targets a protein that controls the cells that break down bone.
8.2 Brain metastases
Whole brain radiotherapy will be offered to people who have a single or small number of metastases in their brain that could be resectable and to those whom surgery is not appropriate [25].
9. Pain relief
There are accessible treatments to effectively control pain during secondary breast cancer. You will initially be given mild pain relief which can then develop to moderate and then strong pain relief when necessary. Morphine-based pain relief has been shown to be effective in controlling many types of pain. Morphine is taken through oral pills, patches or injections under the skin [26]. Some of the most common morphine side effects include sleepiness, constipation and nausea [27].
Doctors often use several other types of drugs to help manage pain. These include:
10. Future treatments
Treatment for advanced ER positive breast cancer is constantly developing. With better understanding of the biology of cancer cells, new therapies can be created. Here we have listed the therapies that are currently being studied.
Advanced Genomic Profiling
In breast cancer, treatment options are decided depending on the presence of oestrogen receptors or HER2 on breast cancer cells. This does not highlight the changes from tumour evolution, causing cases such as the hormone therapy resistance. To allow for more targeted therapies, advanced genomic profiling provides a more in-depth understanding of your breast cancer type. Through rigorously searching your DNA, changes in genes are identified that could make you eligible for different treatments or clinical trials.
Certain changes in genes can make you eligible for a specific treatment. An example of this is in the gene PIK3CA, which makes you eligible for alpelisib (see below). Other findings are not as direct as these, and it is the accruing of various factors that will help decide the best treatment option for you.
If you are not responding to your current treatment, we suggest researching the potential of genomic profiling. Although unavailable on the NHS at present, there are multiple companies that provide the service which can be refundable through healthcare insurance.
Companies providing advanced genomic profiling: Foundation medicine, Guardant360, Claris, Tempus
Anti-TROP2
Initially created to target triple negative breast cancer, anti-TROP2 therapy may have potential in ER+, HER2- breast cancer. The therapy, sacituzumab govitecan, targets TROP-2, which is vital for cancer growth. A study found that this could be a feasible treatment option with response rates comparable to those seen in CDK4/6 inhibitors [28]. Further trials are currently ongoing to compare its benefit compared to chemotherapy after 2-4 previous regimens [29].
Alpelisib (Piqray®) with fulvestrant
A study found that the addition of alpelisib alongside fulvestrant improved overall survival by 8 months. [30] Alpelisib is a type of targeted therapy that targets a certain protein variation present in some types of breast cancer. Normally the protein, called PI3K, helps all cells get the energy they need. If there is a change, then PI3K works a lot quicker than normal, allowing cancer cells to survive and grow. [31]
The inclusion of alpelisib will depend on the presence of this mutation in your cancer cells. It is thought that 40% of HR+, HER2- breast cancer are positive for this mutation. [32]
PARP inhibitors
Another form of treatment tailored to your genetic profile are PARP inhibitors. This treatment is offered to people who are BRCA positive. The most well known of these, olaparib, is currently under review for NHS patients with breast cancer, waiting for the manufacturer to submit new data. At this given time, PARP inhibitors are usually only available on the NHS as part of a clinical trial for people with secondary-breast cancer and an altered BRCA gene.
Combined Immunotherapy
Cancer immunotherapy, which includes monoclonal antibodies such as Herceptin, have been successful in improving survival, however its success have been limited to subsets of the population. MORPHEUS trial is currently studying the effect of combining immunotherapy with chemotherapy or targeted therapy. This is using the drug atezolizumab, a monoclonal antibody, used in triple negative breast cancer and HR+ breast cancer [33].
HDAC inhibitors
A new method of targeting individuals specific breast cancer cells is through inhibiting histone deacetylase. The treatment (HDAC’s), including tucidinostat and entinostat, block the function of histone deacetylase, a protein vital in the process of cell growth. Tucidinostat was found to significantly improve progression-free survival compared to having the aromatase inhibitor exemestane alone. This could pose as a new treatment options for postmenopausal women with advanced breast cancer who have not responded to hormone therapy. However, adverse side effects were noted in 50% of the patients given the drug, and therefore further research is necessary. [34]
And that’s all the treatments summed up for advanced hormone receptor-positive breast cancer. We hope that you now better understand your treatment options and can feel confident in discussions with your care team.
References
[1] O’Shaughnessy, J. (2005). Extending Survival with Chemotherapy in Metastatic Breast Cancer. The Oncologist, 10(suppl_3), pp.20–29.
[2] www.cancer.org. (n.d.). Advanced and Metastatic Cancer. [online] Available at: https://www.cancer.org/treatment/understanding-your-diagnosis/advanced-cancer.html.
[3] Results of the 2014 Realities of living with ABC survey commissioned by Novartis Oncology in the UK with 60 respondents living with advanced breast cancer distributed by Breast Cancer Care.
[4] Results of The Count Us, Know Us, Join Us survey 2013, commissioned by Novartis Oncology in 12 countries with nearly 1 300 total respondents living with advanced breast cancer including 79 in the UK. Conducted by Harris Interactive.
[5] Pan, H., Gray, R., Braybrooke, J., Davies, C., Taylor, C., McGale, P., Peto, R., Pritchard, K.I., Bergh, J., Dowsett, M. and Hayes, D.F. (2017). 20-Year Risks of Breast-Cancer Recurrence after Stopping Endocrine Therapy at 5 Years. New England Journal of Medicine, [online] 377(19), pp.1836–1846. Available at: https://www.nejm.org/doi/full/10.1056/NEJMoa1701830.
[6] Breast Cancer Now. (2018). Secondary breast cancer diagnosis. [online] Available at: https://breastcancernow.org/information-support/facing-breast-cancer/secondary-metastatic-breast-cancer/secondary-breast-cancer-diagnosis [Accessed 26 Oct. 2020].
[7] pathways.nice.org.uk. (7AD). Advanced breast cancer - NICE Pathways. [online] Available at: https://pathways.nice.org.uk/pathways/advanced-breast-cancer [Accessed 26 Oct. 2020].
[8] Taylor, C.W., Green, S., Dalton, W.S., Martino, S., Rector, D., Ingle, J.N., Robert, N.J., Budd, G.T., Paradelo, J.C., Natale, R.B., Bearden, J.D., Mailliard, J.A. and Osborne, C.K. (1998). Multicenter randomized clinical trial of goserelin versus surgical ovariectomy in premenopausal patients with receptor-positive metastatic breast cancer: an intergroup study. Journal of Clinical Oncology, 16(3), pp.994–999.
[9] Mouridsen, H., Gershanovich, M., Sun, Y., Pérez-Carrión, R., Boni, C., Monnier, A., Apffelstaedt, J., Smith, R., Sleeboom, H.P., Jaenicke, F., Pluzanska, A., Dank, M., Becquart, D., Bapsy, P.P., Salminen, E., Snyder, R., Chaudri-Ross, H., Lang, R., Wyld, P. and Bhatnagar, A. (2003). Phase III Study of Letrozole Versus Tamoxifen as First-Line Therapy of Advanced Breast Cancer in Postmenopausal Women: Analysis of Survival and Update of Efficacy From the International Letrozole Breast Cancer Group. Journal of Clinical Oncology, 21(11), pp.2101–2109.
[10] Nice.org.uk. (2009). Recommendations | Advanced breast cancer: diagnosis and treatment | Guidance | NICE. [online] Available at: https://www.nice.org.uk/guidance/cg81/chapter/recommendations [Accessed 26 Oct. 2020].
[11] www.nice.org.uk. (n.d.). 1 Recommendations | Fulvestrant for untreated locally advanced or metastatic oestrogen-receptor positive breast cancer | Guidance | NICE. [online] Available at: https://www.nice.org.uk/guidance/TA503/chapter/1-Recommendations [Accessed 26 Oct. 2020].
[13] Breastcancer.org. (2020). CDK4/6 Inhibitors for Metastatic Breast Cancer: Ibrance, Kisqali, Verzenio. [online] Available at: https://www.breastcancer.org/treatment/targeted_therapies/cdk46-inhibitors.
[14] Turner, N.C., Slamon, D.J., Ro, J., Bondarenko, I., Im, S.-A., Masuda, N., Colleoni, M., DeMichele, A., Loi, S., Verma, S., Iwata, H., Harbeck, N., Loibl, S., André, F., Puyana Theall, K., Huang, X., Giorgetti, C., Huang Bartlett, C. and Cristofanilli, M. (2018). Overall Survival with Palbociclib and Fulvestrant in Advanced Breast Cancer. New England Journal of Medicine, [online] 379(20), pp.1926–1936. Available at: https://www.nejm.org/doi/full/10.1056/NEJMoa1810527.
[15] Im, S.-A., Lu, Y.-S., Bardia, A., Harbeck, N., Colleoni, M., Franke, F., Chow, L., Sohn, J., Lee, K.-S., Campos-Gomez, S., Villanueva-Vazquez, R., Jung, K.-H., Chakravartty, A., Hughes, G., Gounaris, I., Rodriguez-Lorenc, K., Taran, T., Hurvitz, S. and Tripathy, D. (2019). Overall Survival with Ribociclib plus Endocrine Therapy in Breast Cancer. New England Journal of Medicine, [online] 381(4), pp.307–316. Available at: https://cdn.mednet.co.il/2019/10/2019-LEE-BC-Im-et-al-ML-7-OS-NEJM-2019.pdf
[16] Johnston, S., Martin, M., Di Leo, A., Im, S.-A., Awada, A., Forrester, T., Frenzel, M., Hardebeck, M.C., Cox, J., Barriga, S., Toi, M., Iwata, H. and Goetz, M.P. (2019). MONARCH 3 final PFS: a randomized study of abemaciclib as initial therapy for advanced breast cancer. npj Breast Cancer, 5(1).
[17] Sledge, G.W., Toi, M., Neven, P., Sohn, J., Inoue, K., Pivot, X., Burdaeva, O., Okera, M., Masuda, N., Kaufman, P.A., Koh, H., Grischke, E.-M., Conte, P., Lu, Y., Barriga, S., Hurt, K., Frenzel, M., Johnston, S. and Llombart-Cussac, A. (2020). The Effect of Abemaciclib Plus Fulvestrant on Overall Survival in Hormone Receptor–Positive, ERBB2-Negative Breast Cancer That Progressed on Endocrine Therapy—MONARCH 2. JAMA Oncology, 6(1), p.116.
[18] Breast Cancer Now. (2018). Palbociclib (Ibrance). [online] Available at: https://breastcancernow.org/information-support/facing-breast-cancer/going-through-breast-cancer-treatment/targeted-therapy/palbociclib-ibrance [Accessed 26 Oct. 2020].
[19] Baselga, J., Campone, M., Piccart, M., Burris, H.A., Rugo, H.S., Sahmoud, T., Noguchi, S., Gnant, M., Pritchard, K.I., Lebrun, F., Beck, J.T., Ito, Y., Yardley, D., Deleu, I., Perez, A., Bachelot, T., Vittori, L., Xu, Z., Mukhopadhyay, P., Lebwohl, D. and Hortobagyi, G.N. (2012). Everolimus in Postmenopausal Hormone-Receptor–Positive Advanced Breast Cancer. New England Journal of Medicine, 366(6), pp.520–529.
[20] Rugo, H.S., Seneviratne, L., Beck, J.T., Glaspy, J.A., Peguero, J.A., Pluard, T.J., Dhillon, N., Hwang, L.C., Nangia, C., Mayer, I.A., Meiller, T.F., Chambers, M.S., Sweetman, R.W., Sabo, J.R. and Litton, J.K. (2017). Prevention of everolimus-related stomatitis in women with hormone receptor-positive, HER2-negative metastatic breast cancer using dexamethasone mouthwash (SWISH): a single-arm, phase 2 trial. The Lancet Oncology, 18(5), pp.654–662.
[21] Seto, B. (2012). Rapamycin and mTOR: a serendipitous discovery and implications for breast cancer. Clinical and Translational Medicine, 1(1), p.29.
[22]. Nice.org.uk. 2020. NHS England interim treatment options during theCOVID-19 pandemic [online]. Available at: https://www.nice.org.uk/guidance/ng161/resources/interim-treatment-change-options-during-the-covid19-pandemic-endorsed-by-nhs-england-pdf-8715724381
[23].www.nice.org.uk. (n.d.). 4 Evidence and interpretation | Denosumab for the prevention of skeletal-related events in adults with bone metastases from solid tumours | Guidance | NICE. [online] Available at: https://www.nice.org.uk/guidance/ta265/chapter/4-Evidence-and-interpretation [Accessed 26 Oct. 2020b].
[24] www.cancerresearchuk.org. (n.d.). How bisphosphonates work | Cancer Research UK. [online] Available at: https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/bisphosphonates/how-bisphosphonates-work [Accessed 26 Oct. 2020].
[25] www.nice.org.uk. (n.d.). Recommendations | Advanced breast cancer: diagnosis and treatment | Guidance | NICE. [online] Available at: https://www.nice.org.uk/guidance/cg81/chapter/Recommendations#managing-complications [Accessed 26 Oct. 2020c].
[26] Nice.org.uk. (2012). Overview | Palliative care for adults: strong opioids for pain relief | Guidance | NICE. [online] Available at: https://www.nice.org.uk/Guidance/CG140.
[27] Breast Cancer Now. (2015). Pain control and secondary breast cancer. [online] Available at: https://breastcancernow.org/information-support/facing-breast-cancer/secondary-metastatic-breast-cancer/pain-control-secondary-breast-cancer [Accessed 26 Oct. 2020].
[28]. Bardia, A. et al., (2018) Efficacy of sacituzumab govitecan (anti-Trop-2-SN-38 antibody-drug conjugate) for treatment-refractory hormone-receptor positive (HR+)/HER2- metastatic breast cancer (mBC). Journals of Clinical Oncology. 35(15):suppl, 1004-1004
[29]. Clinicaltrials.gov. (2020). Study of IMMU-132 in HR+/HER2- MBC (TROPICS-02). [online] Available at: https://clinicaltrials.gov/ct2/show/NCT03901339 [Accessed 26 Oct. 2020].
[30]. André. F. (2020). LBA18 - Overall survival (os) results from SOLAR-1, a phase III study of alpelisib (ALP) + fulvestrant (FUL) for hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2–) advanced breast cancer (ABC). Annals of Oncology. 31 (suppl_4): S1142-S1215
[31]. Breastcancer.org.(2020). Piqray. [online] Available at: .https://www.breastcancer.org/treatment/targeted_therapies/piqray [Accessed 26 Oct. 2020].
[32]. André, F. et al,. (2019). Alpelisib For PIK3CA-Mutated, Hormone Receptor–Positive Advanced Breast Cancer. New England Journal Of Medicine. 380:1929-1940.
[33]. Yardley DA, Abu-Khalaf M, Boni V, Brufsky A, Emens LA, Gutierrez M, Hurvitz S, Im S-A, Loi S, McCune SL, Schmid P, O'Hear C, Zhang X, Vidal GA. (2019). MORPHEUS: A phase Ib/II trial platform evaluating the safety and efficacy of multiple cancer immunotherapy combinations in patients with hormone receptor–positive and triple-negative breast cancer [abstract]. In: Proceedings of the 2018 San Antonio Breast Cancer Symposium; 2018 Dec 4-8; San Antonio, TX. Philadelphia (PA): AACR; Cancer Res 79(4 Suppl):Abstract nr OT2-06-04.
[34]. Jiang, Zefei et al. (2019). Tucidinostat plus exemestane for postmenopausal patients with advanced, hormone receptor-positive breast cancer (ACE): a randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet Oncology. 20(6):806-815