Although breast cancer is often seen as a women’s disease, men can get it too - and a small number develop secondary (metastatic or advanced) breast cancer. It can feel isolating, but support and treatment are available. Many men find strength in knowing they are not the only ones living with this disease.
On this page you will find:
Understanding secondary breast cancer
Secondary breast cancer happens when cells from the original breast cancer move to another part of the body - often the bones, lungs, liver or brain. It isn’t curable, but it can be treated to help control symptoms, slow progression, and help you live well for as long as possible. Your clinical team will explain your treatment options and work with you to manage side effects and maintain quality of life.
For more information, see Understanding Your Diagnosis.
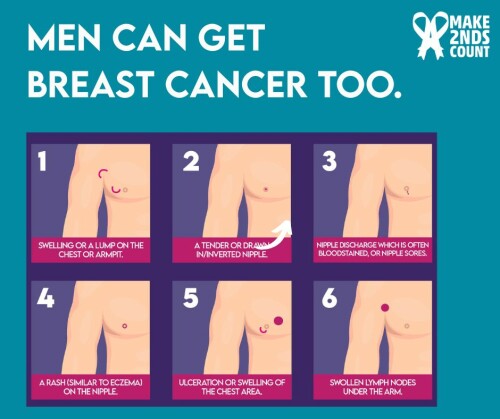
It often starts as a primary breast cancer that has spread over time, though some men are diagnosed at a later stage. Common symptoms are:
-
 Bone pain
Bone pain -
Breathlessness or cough
-
Fatigue
-
Unexplained weight loss
-
New lumps or swelling
-
Nausea
-
Ongoing headaches
Symptoms vary from person to person, and can be dependent on the sites of metastasis, so it is important that you listen to your body and notice anything new. Read more about the signs and symptoms to be aware of here.
Treatment and care
The same principles apply in treating men and women with secondary breast cancer, but treatment plans are tailored for men. Treatments may include:
-
Surgery
-
Hormone therapy
-
Targeted therapies (like HER2 or CDK4/6 inhibitors)
-
Chemotherapy or radiotherapy
-
Immunotherapy
-
Medicines to control symptoms and side effects, such as bone-strengthening drugs or pain management
Every treatment plan is personal. Your team will discuss what’s right for you, explain possible side effects, and support your emotional wellbeing throughout.
For more information, see Treatments.
Body changes and self-confidence
Treatment for secondary breast cancer can bring changes to your body - some are visible, others less so. These changes can affect how you feel about yourself and your sense of identity. It’s completely normal to find this difficult.
You might notice:
-
Changes in weight or muscle tone - hormone therapy can cause weight gain, especially around the chest or stomach, and may make it harder to build or keep muscle.
-
Swelling or tenderness around the chest - surgery, radiotherapy, or medication can lead to puffiness or a swollen area where the breast tissue was removed.
-
Loss of body hair - chemotherapy and some hormone treatments can cause thinning or loss of hair on the head, chest, or face.
-
Hot flushes and sweating - these can be sudden, uncomfortable, and affect your confidence in social or work situations.
-
Changes in energy levels - fatigue is a common side effect and has a significant impact on daily life.
For some men, these changes can affect how masculine they feel, or how comfortable they are with their appearance. You may find yourself avoiding certain clothes, social situations, or intimacy. These feelings are valid and understandable.
It can help to:
-
Talk to your clinical team about managing physical side effects - there may be medication, lifestyle tips, or referrals that can help.
-
Be kind to yourself - your body is going through a lot, and it’s still working hard for you.
-
Consider gentle activity or exercise - it can improve strength, combat fatigue and confidence over time.
-
Speak to someone you trust about how you feel. You don’t have to put on a brave face all the time.
Some men find it reassuring to connect with others who understand what it’s like to live in a body that’s changed because of cancer. You might find it helpful to talk in a support group or online community - sometimes just hearing “me too” can make a big difference.
Sexual wellbeing
It’s common for men with secondary breast cancer to experience changes in their sex life. These can be physical, emotional, or both - and they’re often linked to treatment side effects as well as the stress of living with cancer.
Some treatments, particularly hormone therapy, can lower testosterone levels. This may cause:
-
Reduced interest in sex
-
Difficulty getting or keeping an erection
-
Less intense orgasms
-
Tiredness or a general loss of energy
These effects are physical, not psychological, and they don’t mean you’ve lost your masculinity or that intimacy is no longer possible. Many men find that with time, patience, and the right support, their sex life can adapt in new and positive ways.
If you’re struggling, talk to your clinical team - these issues are very common, and there are ways to help.
-
Medication can sometimes improve erections or manage other side effects.
-
Referral to a specialist clinic may help if hormone or erectile changes are affecting your quality of life.
-
Exercise and maintaining physical activity can also help energy levels and body confidence.
Emotional and relationship changes
Sexual wellbeing isn’t just about the physical side - it’s also about how you feel about yourself and your relationships.
Changes to your body, scarring, or weight can affect confidence or make you feel self-conscious. You might worry your partner will see you differently, or you might avoid intimacy altogether. These feelings are common - and talking about them can help reduce the pressure.
If you have a partner:
-
Try to share how you’re feeling, even if it’s awkward at first.
-
Remember, intimacy doesn’t have to mean sex - closeness, touch, and communication can still bring comfort and connection.
-
Spend some quality time together, just the two of you.
-
If you’re both finding things difficult, couples counselling can help you rebuild confidence together.
If you’re single, you might worry about dating or disclosing your diagnosis. It’s okay to take things at your own pace - you decide when and how to share information about your cancer. Try to remember: your sexuality and self-worth aren’t defined by what your body can or can’t do.
Feeling isolated and dealing with stigma
Because breast cancer is often seen as a women’s illness, many men say they feel invisible or overlooked. It can be hard to find information or images that reflect your experience, and even harder when people seem surprised that a man can get breast cancer at all.
These reactions can make you feel alone, or even reluctant to talk about your diagnosis. Some men worry about what others might think or avoid using the word “breast” altogether. This is completely understandable - but it can also add to feelings of isolation and stigma.
The truth is: breast cancer has no gender. You have just as much right to understanding, empathy, and support as anyone else.
If you’re finding it difficult to talk about your diagnosis, you might try:
-
Sharing how you feel with one trusted person - sometimes just being heard can lift the weight.
-
Talking to your clinical team about your experiences; they’re used to these conversations.
-
Joining a support group or online community - many men find comfort in connecting with others who “just get it.”
Written by Dr Sarah Thomas
Date of last update: October 2025

