20th December 2023 by OWise and Make 2nds Count Education OWiseCollaboration

Aromatase inhibitors are a class of drugs that can be used to treat hormone receptor-positive (HR+) subtypes of breast cancer1. Aromatase inhibitors can be used in the treatment of early HR+ breast cancer, but here we will focus on aromatase inhibitors in treating secondary (metastatic, advanced) breast cancer. We will cover how they work, who they are for, clinical data, side effects to look out for, and the experience of three secondary breast cancer patients who are on aromatase inhibitor drugs. This blog was written in collaboration with OWise.
Aromatase inhibitors (AIs) are a type of hormone (endocrine) therapy that can be prescribed to treat both primary and secondary HR+ breast cancer. To date, three generations of AIs have been developed. There are currently several third-generation AIs available, including:
In HR+ breast cancer the cancer cells grow in response to the hormone’s oestrogen and/or progesterone. For pre-menopausal women, the main source of oestrogen and progesterone is from the ovaries. In post-menopausal women, main source of oestrogen is from the aromatase pathway once periods have stopped.
The aromatase pathway is where androgens (sex hormones created in the adrenal glands and ovaries) are converted into oestrogens. Aromatase is the enzyme responsible for the conversion of androgens into oestrogens (figure 1). This happens all over the body including in the fat, liver, muscle or brain cells.
AIs block the aromatase enzyme from converting androgens into oestrogen, thereby lowering the levels of oestrogen in the body (figure 1). This can result in a decrease of circulating oestrogen to undetectable levels, thereby reducing growth of cancer cells that are fuelled by oestrogen.
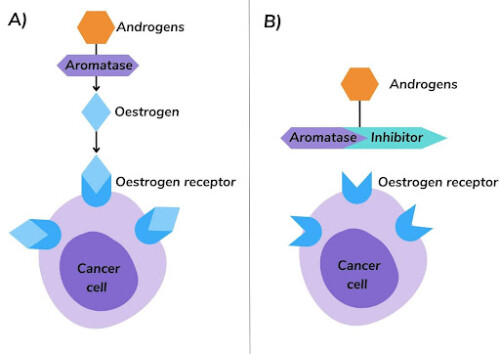
Figure 1. A) Aromatase converts androgens to oestrogen that binds to oestrogen receptors on cancer cells. B) Aromatase inhibitors prevent the conversion of androgens to oestrogen, reducing the amount of oestrogen available to bind to oestrogen receptors on cancer cells.
AIs are available to treat secondary breast cancer in3:
AIs can also be used in3:
The PO25 trial compared letrozole with tamoxifen in post-menopausal women with secondary HR+ breast cancer. Results found that for most patients the cancer did not worsen or spread for 9.4 months while on letrozole, compared to 6 months on tamoxifen4 (figure 2).
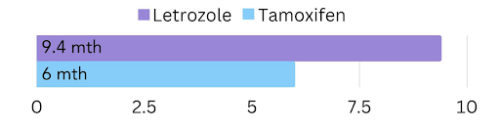
Figure 2. The amount of time cancer did not worsen or spread in post-menopausal women with secondary HR+ breast cancer on letrozole vs. tamoxifen. Additionally, the data suggested that letrozole improved survival for most patients by 14 months compared with tamoxifen4.
A trial compared anastrozole with tamoxifen in post-menopausal women with secondary HR+ breast cancer. It was found that for most patients on anastrozole the cancer did not worsen or spread for 18 months, compared to 7 months on tamoxifen5 (figure 3).
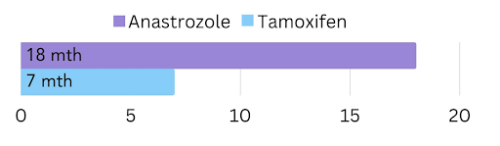
Figure 3. The amount of time cancer did not worsen or spread in post-menopausal women with secondary HR+ breast cancer on anastrozole vs. tamoxifen. At the end of the trial 40% of patients on anastrozole were alive, compared to 11% on tamoxifen5.
Exemestane was compared with tamoxifen in post-menopausal secondary HR+ breast cancer patients. Results found that in 46% of patient the cancer responded to treatment (decrease in tumour size or disappearance of all signs of cancer) while on exemestane, compared to 31% on tamoxifen6 (figure 4).
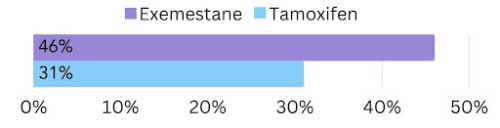
Figure 4. The amount of post-menopausal women with secondary HR+ breast cancer that responded to exemestane vs. tamoxifen treatment. Additionally, data suggested that the amount of time on average patients lived without the cancer worsening (median progression free survival) was 9.9 months with exemestane, compared to 5.8 months with tamoxifen. However, looking at the results over a longer period, the progression free survival and survival was similar with exemestane and tamoxifen6.
AIs can be combined with other treatments, such as CDK 4/6 inhibitors. CDK 4/6 inhibitors are a class of oral drugs that inhibit proteins called CDK4 and CDK6, these proteins are important in cell division. Abemaciclib (Verzenio®), palbociclib (Ibrance®) or ribociclib (Kisqali®) in combination with an AI are recommended as a first-line treatment for previously untreated secondary breast cancer3.
Clinical trials have demonstrated that most patients being treated with a CDK 4/6 inhibitor in combination with an AI live around 10 months longer on average, compared to patients being treated with an AI alone7,8,9.
As with all medications, AIs can cause side effects. Many of these side effects are symptoms of menopause, such as joint pain, hot flushes and vaginal dryness. Another side effect of AIs is thinning or weakening of the bones, also known as osteoporosis. It is important to monitor these side effects and share your symptoms with your care team if they are negatively impacting your life.
Joint pain caused by AIs is most commonly experienced in the fingers, wrists, shoulders, knees and ankles. It can begin at approximately 2 months after the start of treatment and to peak at around the 6-month mark, but it can appear up to 2 years after initiation of therapy. There are some methods that can manage joint pain:
Hot flushes (flashes) are characterised by a sudden sensation of intense, internal heat in the chest, face and head. This feeling may be accompanied by flushing, sweating and chills. Many people get hot flushes at night and can make it difficult to get a good rest, which can result in mood changes and feeling irritable. Try some of the following tips to manage hot flushes:
Vaginal dryness is a symptom of vulvovaginal atrophy (VVA), which is strongly associated with low oestrogen levels. This symptom is often underreported and can have an impact on sexual function and quality of life. Try the following to improve vaginal dryness symptoms:
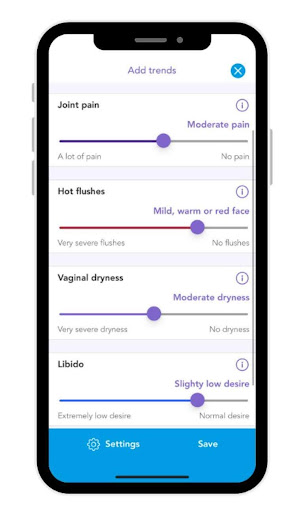
With OWise you can monitor side effects caused by aromatase inhibitors, such as joint pain, hot flushes and vaginal dryness. You can visualise how your trends over time and share these trends directly with your care team.
Oestrogen is involved in maintaining healthy bones in men and women10. As AIs lower the levels of oestrogen in the body they can increase the risk of osteoporosis, thereby increasing the risk of fracture. It is important to be aware of the following:

I was diagnosed with a stage 4 cancer back in December 2022 having been suffering liver and back pain for a couple of months. It had the unusual presentation of there being no evidence of disease in my breasts, hence the long delay to diagnosis and me residing in cancer of unknown primary. A very scary time. I was actually relieved to get the diagnosis as horrendous as it was.
I started letrozole treatment on 17 February 2023, having stopped hormone replacement therapy (HRT) back in December 2022. I had never had any other previous medication for anything. The mere stopping of HRT reduced my liver lesions by half. I started abemaciclib (Verzenio®), a CDK 4/6 inhibitor, one month later.
I am no stranger to the effects of the menopause and lack of oestrogen as I entered the menopause at the age of 56. At that time, the lack of oestrogen was very debilitating, so I wasn’t looking forward to starting letrozole and zoladex, to shut my ovaries down, a double whammy. Generally, it has been fine and nowhere near as bad as my first menopausal experience.
It’s hard to know which side effects are caused by the aromatase inhibitor. I do experience a hot flush or two but nowhere near as bad as before and usually about an hour after taking it. Initially I had quite a lot of pain in my joints and felt older than my age. I’ve always been fit but it was an effort for a little while. I can honestly say that I don’t really get that anymore unless I’ve been gardening and bending down a lot.
I recently had my cholesterol tested and it was really high so I’m investigating that, although my blood pressure is good. Possibly a side effect, but my family history is not great on that front. I have had problems with watery eyes and have a residual chalazion on my eye as a result – it is disappearing slowly.
My hair is thinning. I had a very thick head of long hair but it is falling out. Not sure if I’ll lose it all. Generally, I sleep well with occasional wakefulness but often that is more about my thought processes beginning when they shouldn’t. I’m learning to shut these out. I have vaginal atrophy which worries me quite a lot but it’s very difficult to get good answers/help from the medical profession. Sex is out of the question and that is a big loss to me.
Some of the above side effects may be from the abemaciclib, zoladex or denosumab.
I’ve not been on OWise long, but I have found it really useful to log symptoms and how I feel so that I can pinpoint the cause of side effects and check to see if there was a pattern. I had previously been using an Excel spreadsheet.
It’s a boon being able to work from home most of the time and perhaps that is why the side effects aren’t as bothersome as they could be. I take letrozole at night not long before bed and I leave two hours between drugs if I can. I take my evening abemaciclib at 6:30 and my Letrozole at 8:30 so I can have a little hot flush to keep me warm whilst watching telly. Occasionally, I wake up with one and fling the covers off. Winter is my friend.
As for the eye watering, I have Hypromellose drops as strangely your eyes get dry and sore. I also use eye masks that I can heat in the microwave and I make sure to bathe my eyes in warm sterile water. I eat healthily and try and make sure I make up for any deficiencies I see in my blood tests. I do lots of weight bearing exercises – I own horses so that’s not difficult!
I also find that even if I am a bit tired, a good walk really invigorates me, so I try to fit one in every day.
I try to do stretches – they really helped with hip pain that I suffered when I was riding horses. I would do them before and after and eliminated the pain. I have been prescribed Replens for vaginal dryness by the doctor, but it’s never available at the pharmacy so I must try and get a substitute.

I was diagnosed HR+/HER2- de novo (so straight to a secondary diagnosis, with no history of primary breast cancer) in November 2020. It was a complete shock to go from ‘hmm…something doesn’t look quite right’ to ‘you have incurable cancer’ in the course of about three weeks.
My first treatment was letrozole with another drug, palbociclib (Ibrance®), a CDK 4/6 inhibitor. I took this combination of drugs for around two and a half years, until the cancer started to spread again in March 2023. After a short break on another type of drug which didn’t work, I am now taking a different aromatase inhibitor, exemestane, alongside everolimus (an mTOR inhibitor).
One of the big advantages of the aromatase inhibitors that I’ve taken is that they are a single tablet that you take once a day – although you have to take exemestane with food. That makes them pretty straightforward to manage.
While I was on letrozole, I found my joints got very stiff – especially my ankles. Sometimes I felt like a penguin waddling about…and I am generally pretty fit. It was only after I stopped taking letrozole that I realised how stiff it had made me feel.
I also had a lot of hot flushes with letrozole, although some brands of medication seemed worse than others, so that could be attributable to ‘fillers’ rather than letrozole itself. I also had some hair thinning in the first few months, but I’m not sure how much that was caused by letrozole and how much by palbociclib.
As a combination, exemestane and everolimus have a lot more side-effects than letrozole and palbociclib, and it’s more difficult to point the finger of blame at one or the other! I haven’t experienced as many hot flushes and my joints haven’t felt quite as stiff as with letrozole – but I’ve only been taking exemestane for four months, rather than the two and a half years that I had on letrozole.
The exemestane/everolimus combination has taken a lot of getting used to. I felt quite grim – tired, struggled to concentrate and nauseous - for the first couple of months that I took it, but it has settled down.
I’ve found that I need an afternoon nap on this combination (exemestane and everolimus) and I need to be more careful about managing my energy overall as I get tired more easily.
Here’s my four tips for managing life on aromatase inhibitors:

In November 2016, I went to see my GP with a variety of symptoms as I just wasn’t feeling right. At that appointment my GP said that my IBS (irritable bowel syndrome) had flared up. At the subsequent monthly appointments that I had with my GP, IBS was the diagnosis, until March 2017.
After a CT scan and resultant breast biopsy, I was diagnosed with Primary Breast Cancer in July 2017. A 12mm growth was found in my left breast and a liver growth, the MDT (Multi-disciplinary team), diagnosed this as benign. After I was diagnosed with MBC, it was clear that this was the cause of the IBS-like symptoms I had been suffering since 2016.
I was offered, and had, a lumpectomy in August 2017. During the surgery, lymph nodes were removed and after testing were negative of any cancer cells, so I continued to be treated as a stage 1 breast cancer patient.
In October 2017, after recovering from surgery, I started four weeks of daily radiotherapy. Part way through this treatment, I had a further CT scan to check on my benign liver growth. Due to its size at the initial CT scan earlier on in the year, I was told it could still cause issues even though it was benign. This scan showed that the tumour had grown, so I was informed that it needed to be biopsied to check its histology. In November after the biopsy, I was told that the I had metastatic breast cancer and that it had spread to my liver.
After my mis-diagnosed primary diagnosis, I was initially started on tamoxifen and remained on this until the December. In December 2018 I started on zoladex and letrozole. In January 2018, after the zoladex had put me into early menopause, I started on palbociclib 125mg alongside letrozole and Accrete D3 (to prevent and treat vitamin D and calcium deficiency).
Since starting palbociclib, I have had the dosage reduced and am now on 75mg.
I switched from letrozole to exemestane in 2021 due to the increasing awful side effects. Since June of this year (2023), I now alternate between letrozole and exemestane to try and minimise the side effects.
Side effects I have experienced because of letrozole are numerous, and I have probably missed a few! These are not in order of severity. Hair thinning/loss, hair breaking, weight gain, dry skin, dry eyes, watery eyes, brittle nails, vision changes, joint pain, muscle aching, total body stiffness, hot flushes, mood changes, loss of libido, vaginal dryness, leg cramping, fatigue, tiredness, headaches, brain fog.
The side effects from letrozole increased and increased, to the point where my oncologist suggested switching over to exemestane. Prior to this change, my oncologist gave me a break from letrozole to allow it to complete leave my system and to confirm that it was this drug that was causing the issues, and not palbociclib or arthritis.
It took 9 weeks for this to happen, and at this point the difference in how I felt was staggering. Before this break, I was at the stage where I was crawling up the stairs on my hands and feet due to the horrendous stiffness and pain, and I was suddenly able to walk up the stairs relatively normally!! And this wasn’t the only improvement I felt not being on the drug, all the others seemed to ease.
At week 12 I started exemestane. The majority of the side effects I had with letrozole restarted after I began taking exemestane, although each of these were at a lower level than previously. Unfortunately, as with Letrozole, the side effects started to get worse and worse. My oncologist suggested alternating between the two drugs, to hopefully minimise the side effects. I started this new drug pattern in June, and I’m hoping that once I settle into this new alternating cycle, my side effects will stabilise at a manageable level.
I have not found anything (increase in exercise regime, diet changes, alternative therapies etc) that have made any significant effect on the side effects I experience from letrozole/exemestane. I am hoping that switching between the two of these aromatase inhibitors will help reduce some of the side effects.
My advice is to listen to your body, if you feel you have the energy to do something you enjoy, grasp it with open arms. And then when your body is telling you to rest, do it!
AIs offer an effective treatment option for secondary HR+ breast cancer in post-menopausal women, or in some cases pre-menopausal women and men. Clinical evidence has demonstrated that in most cases aromatase inhibitors result in improve outcomes compared to tamoxifen, and that AI treatment combined with a CDK 4/6 inhibitor is more effective than AI treatment alone. Side effects may occur, but open communication with the care team can help patients to manage these challenges and improve outcomes.
At OWise, we want to make sure you are kept informed so make sure to follow our Instagram and Facebook for any updates. Any questions? Get in touch!