19th July 2023 by OWise Education OWiseCollaboration

Secondary breast cancer (also known as metastatic, stage 4 or advanced breast cancer) occurs when the cancer spreads beyond the breast and nearby lymph nodes to other parts of the body.
In this blog we will share information on secondary breast cancer, metastases, the signs to look out for, and the diagnosis of secondary breast cancer. This blog features as part of a series collaboration with Make 2nds Count, so be sure to check out some of the other blogs too!
A recent audit of NHS England data estimates that the number of patients living with secondary breast cancer in England was over 57,000 in 20211. As UK wide data on the number of patients living with secondary breast cancer is not centrally collected or reported, an entire UK estimate is difficult to obtain1.
Secondary breast cancer can happen when cancer cells from the primary (original) tumour spread to other parts of the body, this process is called metastasis2. Most commonly, these cells can spread to the liver, lungs, bones, and brain3. These cancer cells can then grow at these new sites and form secondary (new) tumours.
Invasive ductal carcinoma (IDC) is the most common type of invasive breast cancer and starts in the milk ducts of the breast. Cancer cells can break through the wall of the milk duct and begin growing into nearby breast tissues. From here the cancer cells can spread through the lymphatic system and bloodstream to other parts of the body4. IDC most commonly metastasises to the bones, lungs, brain and liver5.
Invasive lobular carcinoma (ILC) is another common invasive breast cancer that begins in the breasts milk producing glands (lobules). ILC can metastasise to the same sites as IDC, as well as the gastrointestinal tract, reproductive organs, abdominal lining, as well as other sites6. Unfortunately, the risk of primary breast cancer metastasising is not fully understood or easy to predict7.
There has been a lack of data on the number of people living with secondary breast cancer. Without data being collected it was estimated in 2019 that around 35,000 people were living with secondary breast cancer in the UK. After years of campaigning by several breast cancer charities including Breast Cancer Now, the NHS announced they would commission an audit in England and Wales in 20218. Data from an audit of NHS England data has resulted in the estimate that over 57,000 patients are living with secondary breast cancer in England in 20211.
Metastasis is when cancer cells spread to other sites in the body. Any new tumours that grow at new sites are called metastases, which is the plural term for metastasis9. For metastases to develop, cancer cells must go through a complicated process, this is referred to as the metastatic pathway (Figure 1). It involves the following steps10:
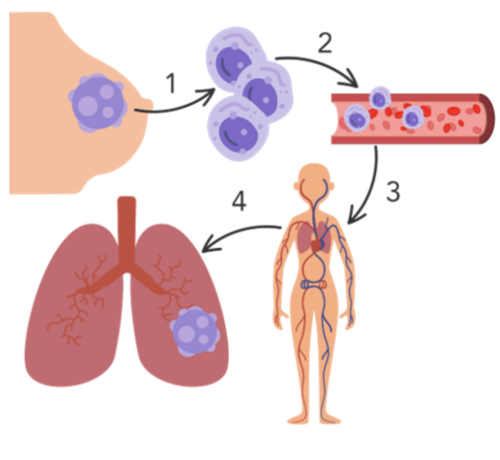
Figure 1. The metastatic pathway: 1) Cancer cells detach from the primary tumour site and invade the surrounding area of normal tissue 2) cancer cells invade the blood or lymphatic system 3) cancer cells travel through the blood or lymphatic vessels to reach target sites 4) cancer cells exit the blood or lymphatic vessels and form a secondary tumour at the target site e.g. the lungs.
During this process many cancer cells often die along the way10,11. However, if conditions are right at each step of the process, cancer cells may be able to form tumours at new sites in the body. Once cancer cells reach a secondary site they do not always turn into aggressive tumours, they can stay inactive for a while, or permanently12.
There is increasing evidence that indicates it is possible for some patients to have limited metastatic disease, known as oligometastatic disease. This is considered an intermediate stage between the primary tumour and widespread metastatic tumours. Research suggests oligometastases can potentially be cured with aggressive local treatment, such as surgery or radiotherapy13. This is a relatively new concept, and the exact definition and treatment approach can vary, but it usually means having a small number of metastases (usually less than five) in few organs.
It is important to be aware of the signs and symptoms of secondary breast cancer, although they can vary from person to person. Some general symptoms to be aware of include fatigue, loss of appetite, weight loss and depression14. Depending on where the cancer has spread to there are more specific symptoms to look out for, these include:
If you are concerned about any symptoms, you should get them checked by your GP or during a check-up appointment. It can be helpful to track these symptoms to share with your doctor.

Do you know that you can track more than 30 side effects and symptoms with OWise? You can monitor any changes and share these with your care teams and loved ones. Better communication with your care team can ensure you receive the best care possible.
For the key signs to look out for IDC and ILC secondary breast cancer, take a look at the infographics made by ABC Diagnosis16.
Medical imaging techniques are tests that can be done to see if the cancer has spread. These tests are helpful for your care team to understand how far and where the cancer has spread. Some commonly used imaging techniques include:
A tumour biopsy helps your care team to understand characteristics of the metastatic breast cancer. It involves a small sample of tissue being taken from the secondary tumour and looking at it under a microscope. The sample can be taken from many parts of the body, including lymph nodes, lungs, liver, bone, skin or bodily fluids22. We have a blog to help with understanding your pathology report.
In metastatic breast cancer, tumour biopsies are done to check if the features of the cancer have changed since the primary diagnosis. The cancer cells in the secondary tumour might have different features compared to the primary tumour, such as oestrogen receptors (ER), progesterone receptors (PR), and human epidermal growth factor receptor 2 (HER2) present on the cell surface23. This is important information as treatment decisions based on the receptors of the primary breast cancer may not always be suitable for the treatment of the secondary breast cancer.
Although tissue biopsies are more common, it is also possible to have a liquid biopsy. This involves taking a sample of bodily fluid (e.g. blood, saliva) to detect and analyse cancer cells or cancer cell DNA. Liquid biopsies can find genetic mutations in cancer cells, see if certain treatments are suitable, and monitor how well treatment is working22. They are useful when a tissue biopsy cannot be done or when quick results are needed. However, results from a liquid biopsy are often used along with tissue biopsy results to guide the treatment decisions.
It is important to note that in some cases patients can be diagnosed with secondary breast cancer at the initial diagnosis,this is called de novo metastatic breast cancer24,25. It was found that 3.8% of women were diagnosed with de novo metastatic breast cancer, compared to 5.8% of men24,25. Male breast cancer forms 1% of all breast cancer diagnoses but their breast cancer is often diagnosed at later stages24,25. Tissue biopsies are useful in this scenario to determine the features of the cancer and develop a treatment strategy.
Molecular testing involves testing a biopsy sample for biomarkers that are associated with cancer growth and spread. These biomarkers can include genes, proteins, or other material. This may provide further insights about what characteristics could be targeted with treatment (Table 1).
Tumour genomic tests can be used to measure the expression of certain genes in a biopsy sample. Measuring the expression of genes is useful to determine how likely a gene is to affect the behaviour of the cancer, including how likely it is to grow and spread.
For secondary breast cancer, genetic tests such as next generation sequencing (NGS) or sequencing panels are being developed. These tests can provide information about the weaknesses or vulnerabilities of the tumour. They can also help determine if certain changes in genes can make a person eligible for specific treatment. For example, a mutation in the PIK3CA gene could make a secondary HR+/HER2- patient eligible for treatment with alpelisib (Piqray®, Table 1).
Although secondary breast cancer cannot be cured, there are treatment options that can help to manage the spread of the cancer, improve quality of life, and maintain overall health and wellbeing26. The treatment approach depends on factors such as the type of breast cancer, where it has spread, genetic factors, and previous treatments received. Keep an eye out for our later blog posts in this series for more information on specific treatment options for secondary breast cancer.

Secondary breast cancer presents unique challenges for breast cancer patients, as it involves the spread of cancer cells from the breast to other parts of the body. While secondary breast cancer cannot be cured, advancements in treatment options offer hope for managing the disease and improving quality of life. By staying informed and seeking appropriate medical care, patients can navigate the complexities of secondary breast cancer with confidence.
At OWise, we want to make sure you are kept informed so make sure to follow our Instagram and Twitter for any updates. Any questions? Get in touch!